Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammatory back pain (IBP) is the core symptom in patients with axial spondyloarthritis (axSpA). For its assessment, experts recommend using the Assessment of SpondyloArthritis International Society (ASAS) criteria. Advances in telemedicine and online screening strategies require to evaluate whether self-reported perform equally to physicians’ assessment.The objective of this study is to assess the agreement and correlation between self-reported and physician´s assessments of ASAS IBP criteria and evaluate their performance compared with rheumatologist´s judgement for IBP.
Methods: The “Strategy for a Hospital Early Referral in Patients with Axial Spondyloarthritis” (SHERPAS) is a prospective ongoing study recruiting young patients (18 to 40 years) with chronic back pain asked to undergo an MRI of the spine by other specialists different than rheumatologists in a tertiary hospital, starting in September 2021. After inclusion, an additional MRI of the sacroiliac joints (SIJ), followed by a rheumatology visit and eligible blood tests were performed. IBP was assessed in 3 different independent ways: i) ASAS criteria asked verbatim by the rheumatologist (ASAS-IBP-phy criteria), ii) ASAS criteria embedded in a self-reported questionnaire (ASAS-IBP-self reported), and iii) according to rheumatologist judgement in the interview (IBP-rheumatologist). Dataset for this interim analysis was locked in October 2022. Kappa statistic (κ) and tetrachoric correlation coefficient (rt) were calculated to assess the agreement and correlation between ASAS-IBP-phy criteria and ASAS-IBP-self reported. Overall accuracy, sensitivity, specificity, positive and negative predictive values for each IBP assessment method were calculated, using IBP-rheumatologist as gold standard.
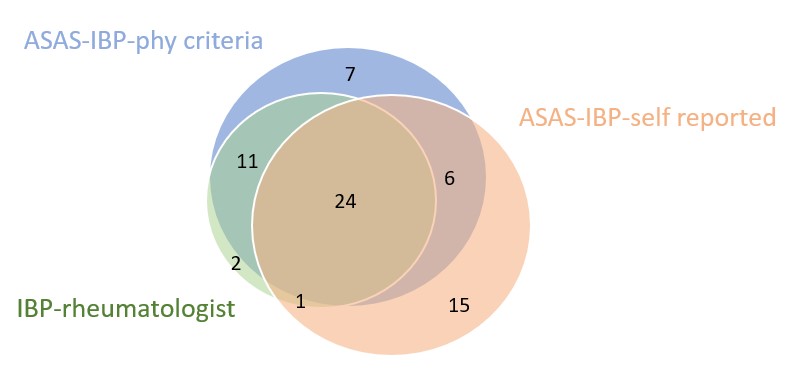
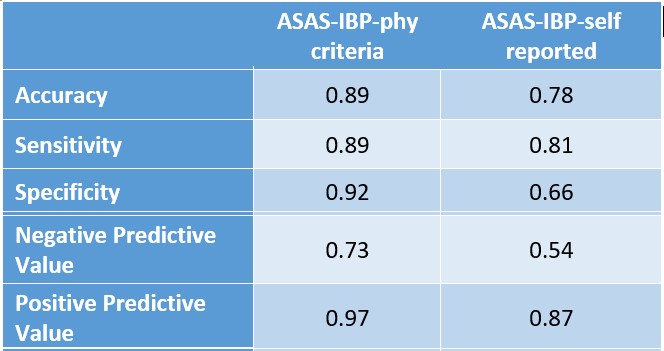
Results: Among 152 recruited patients, 85 (55.9%) were female; mean (SD) age was 34.2 (5.3) years. 66/152 (43.4%) patients reported IBP by at least one of the three assessments, and 24 (15.8%) patients presented back pain as assessed by the three methods altogether. Venn diagrams representing the overlap between the different IBP assessments are shown in Figure. A moderate agreement (κ =0.48) and strong correlation (rt=0.7) were found between ASAS-IBP-self reported and ASAS-IBP-phy criteria. While ASAS-IBP-phy criteria showed a strong level of agreement and very strong correlation with IBP- rheumatologist (κ = 0.74, rt= 0.94), ASAS-IBP-self reported showed a moderate agreement and moderate correlation with this outcome (κ = 0.44, rt=0.67). ASAS-IBP-phy criteria showed better performance than ASAS-IBP-self reported for capturing IBP- rheumatologist [accuracy of 0.89 (95%CI 0.83- 0.94) vs 0.77 (95%CI 0.70- 0.84)] (Table).
Conclusion: ASAS criteria to define IBP show higher level of agreement and correlation with IBP rheumatologist overall judgement when assessed by physician as compared to a self-reported assessment. These results call for caution when extrapolating use of experts IBP criteria from clinical to online setting and suggest that clinicians should prioritize physician assessment over self-report to define this.
To cite this abstract in AMA style:
Benavent D, Tapia M, Bernabeu D, muley V, Plasencia-Rodríguez C, Balsa A, Navarro-Compán V. Self-Reported and Physician´s Assessment of Inflammatory Back Pain According to ASAS Criteria: Is It the Same? [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/self-reported-and-physicians-assessment-of-inflammatory-back-pain-according-to-asas-criteria-is-it-the-same/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-reported-and-physicians-assessment-of-inflammatory-back-pain-according-to-asas-criteria-is-it-the-same/