Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Lack of timely rheumatology referral for suspected axial spondyloarthritis (axSpA) is a major contributor to delayed diagnosis in patients with chronic back pain (CBP). Poor disease awareness among non-rheumatologists and busy practice patterns adversely affect referral process. In ongoing Finding Axial Sponyloarthritis (FaxSpA) study, we are evaluating the effectiveness of a self-referral strategy where the screening tool is directly distributed to at risk patients using electronic medical record and social media.
Methods: In a prospective single center study, we developed a screening tool (A-tool) that consists of 3 question prescreen and 8 question screening questionnaire (SQ). Patients who pass all questions in prescreen can access the SQ. A-tool is considered positive in case of 3 or more positive responses to SQ. A-tool is distributed online via patient portal (Mychart) to those age 18 to 65 yr with CBP listed on the problem list. A-tool is also distributed via Facebook to those in our geographical area. Patients with positive A-tool are contacted to confirm eligibility and are invited for a visit. Patients with known diagnosis of axSpA, age >65 yr and previous spine surgery are excluded. Patients undergo history and physical, labs (CRP and HLA-B27) and imaging studies (X-ray and MRI of pelvis). Clinician’s judgement is considered gold standard for diagnosis of axSpA. DNA and plasma samples are stored for biomarker research. Statistical analysis was done with descriptive statistics, T-test and chi-square tests.
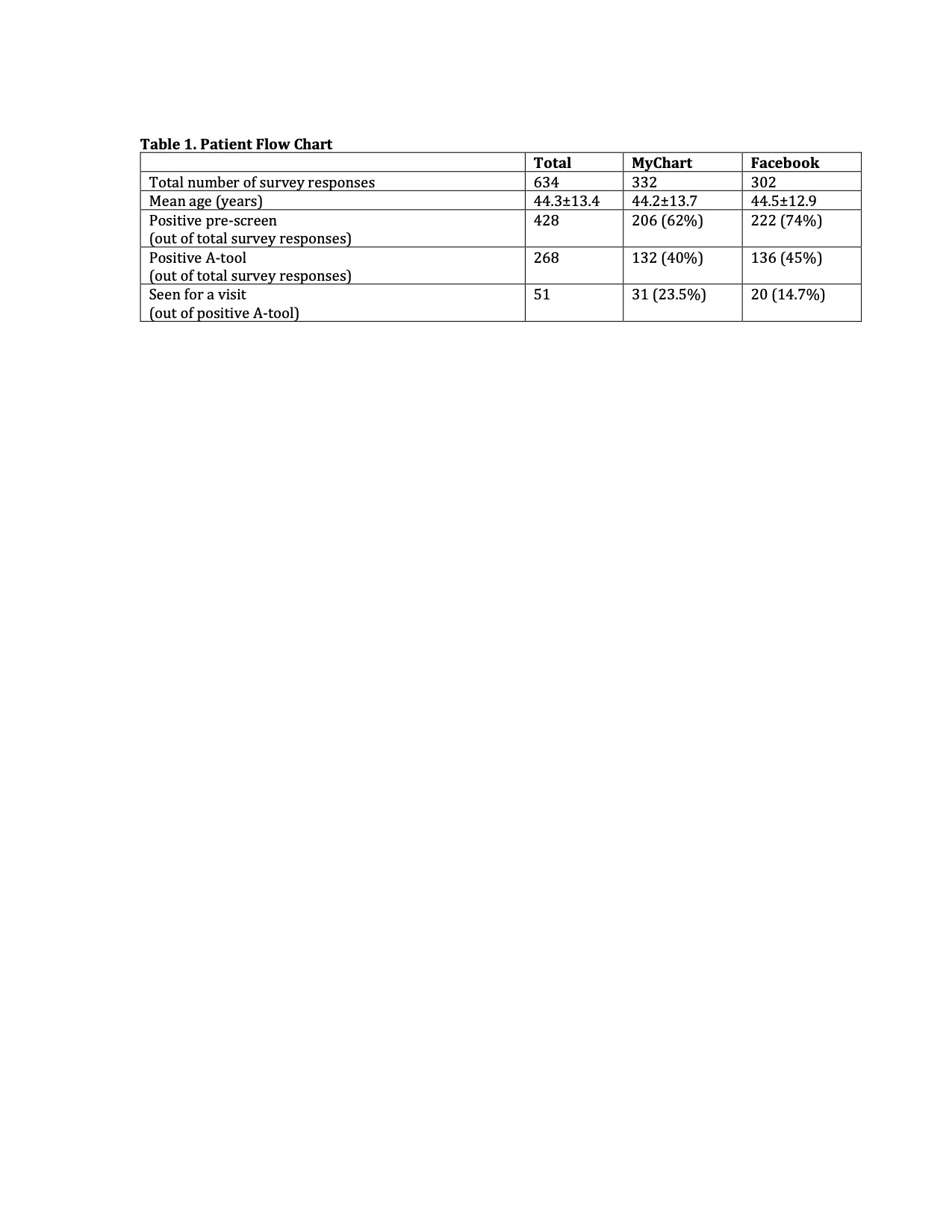
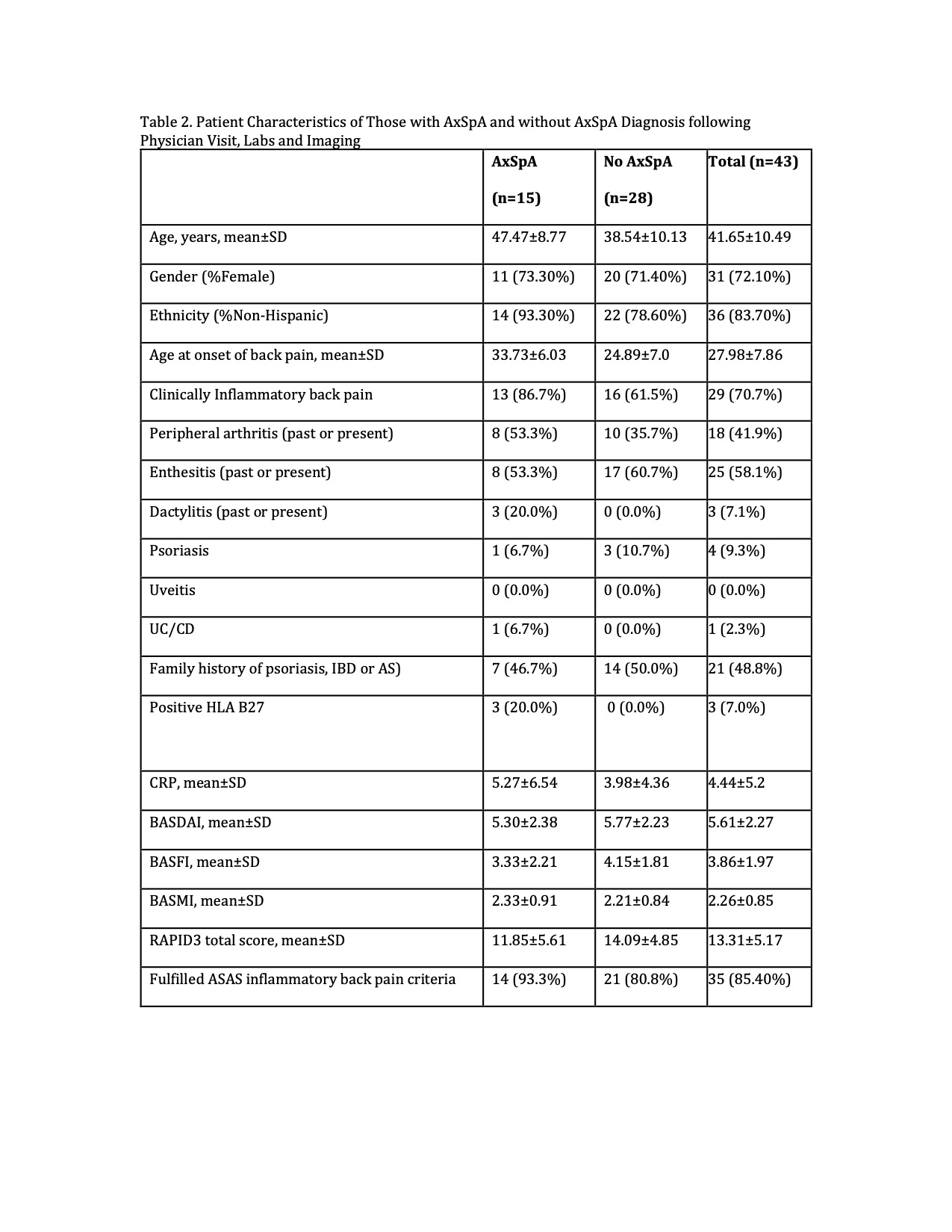
Results: Total 634 patients took the survey through MyChart (52%) or Facebook (48%) from April 2019 to March 2020 (Table 1). Among the responders, 428 (68%) had positive pre-screen and 268 (42%) had positive A-tool. We were unable to reach 90 subjects. Sixty-seven were ineligible after a phone interview (11 had confirmed axSpA, 15 had previous surgery, 18 changed answers to A-tool). Another 38 were unable to come or were no longer interested. As of November 2020, 51 patients came for study visit and 43 completed labs and imaging. Out of 43 patients, 15 (34.9%) were diagnosed with axSpA (6 with AS and 9 with nr-axSpA) (Table 2). There was a trend suggesting that as the number of positive responses on SQ increases, likelihood of axSpA diagnosis was greater.
Conclusion: Our preliminary findings suggest that A-tool based self-referral strategy for early diagnosis of axSpA among patients with CBP is practical and feasible approach. We need larger prospective study to validate our findings and confirm the effectiveness of the A-tool based referral strategy.
To cite this abstract in AMA style:
Afinogenova Y, Alexander S, Haims A, Danve A. Self-referral Strategy for Early Diagnosis of Axial Spondyloarthritis- Preliminary Analysis from Finding Axial Spondyloarthritis Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/self-referral-strategy-for-early-diagnosis-of-axial-spondyloarthritis-preliminary-analysis-from-finding-axial-spondyloarthritis-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-referral-strategy-for-early-diagnosis-of-axial-spondyloarthritis-preliminary-analysis-from-finding-axial-spondyloarthritis-study/