Session Information
Date: Tuesday, November 12, 2019
Title: Pediatric Rheumatology – ePoster III: Systemic JIA, Fever, & Vasculitis
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Macrophage Activation Syndrome (MAS) is a severe, life-threatening, complication of rheumatic diseases in childhood, particularly of systemic Juvenile Idiopathic Arthritis (sJIA), occurring in approximately 25% of the patients with sJIA. The mortality rate of MAS is still significantly high. A score that identify sJIA patients who are at high risk to develop MAS would be useful in clinical practice. There are no parameters available to identify from onset sJIA patients with high risk to develop MAS in their disease course.
Methods: We evaluated whether routine laboratory parameters at disease onset may predict the development of MAS in patients with active sJIA and we defined a risk score of MAS for sJIA patients using these parameters. Laboratory parameters of disease activity and severity (WBC, N, PLT, Hb, ferritin, AST, ALT, gGT, LDH, TGL, fibrinogen, D-dimer and CRP), were retrospectively evaluated in 85 sJIA patients referred to our Division of Rheumatology from 1998 to 2018 with at least one year of follow-up. Laboratory parameters were evaluated during active sJIA, without MAS, at time of hospitalization (T1) and immediately before treatment for sJIA was started (T2). Patients were divided in two groups: group 1 (sJIA patients without history of MAS), group 2 (sJIA patients with at least one MAS episode during disease course). To calculate a MAS risk score, laboratory parameters, collected at T2, with a statistically significant difference between the two groups of patients were selected.
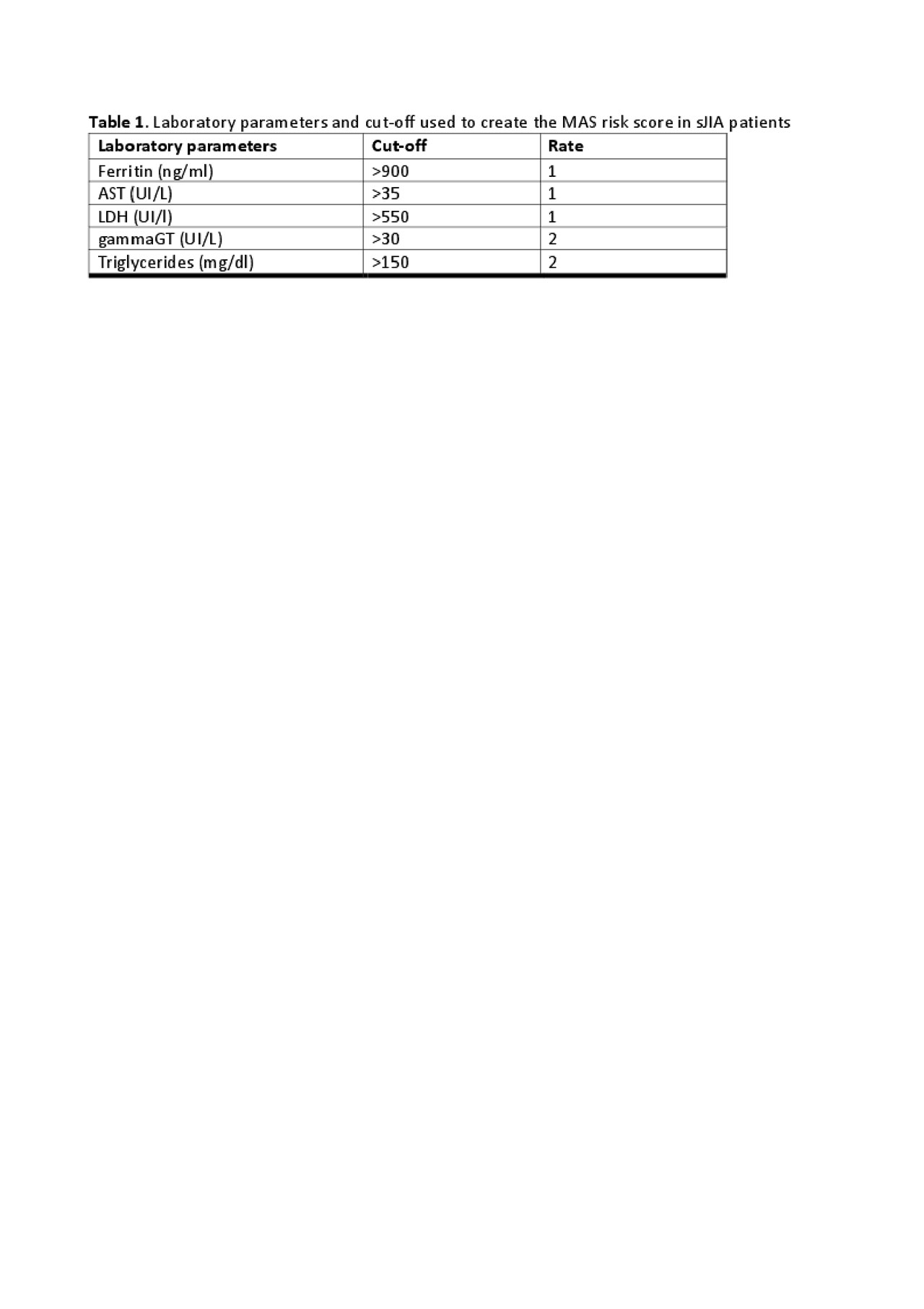
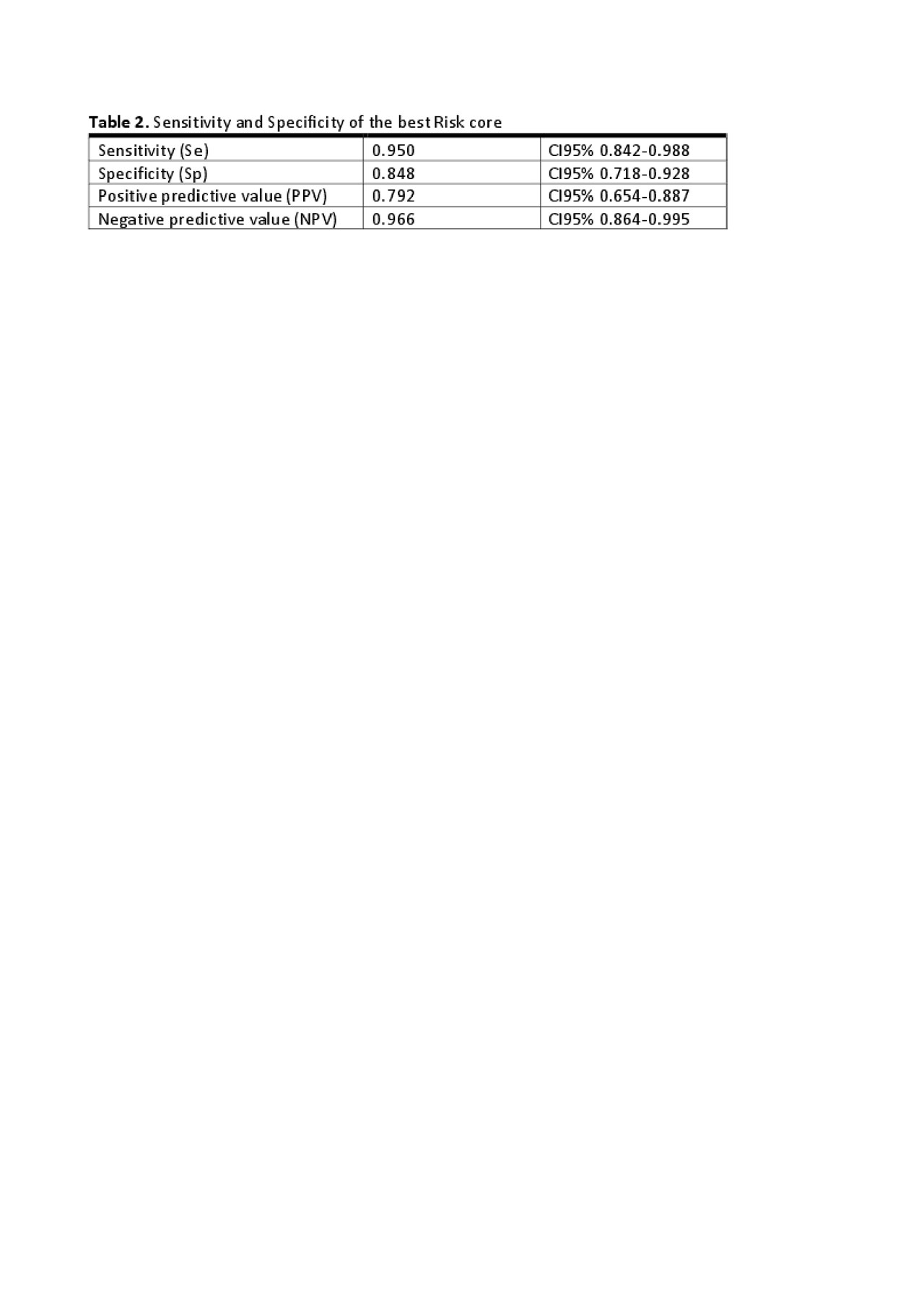
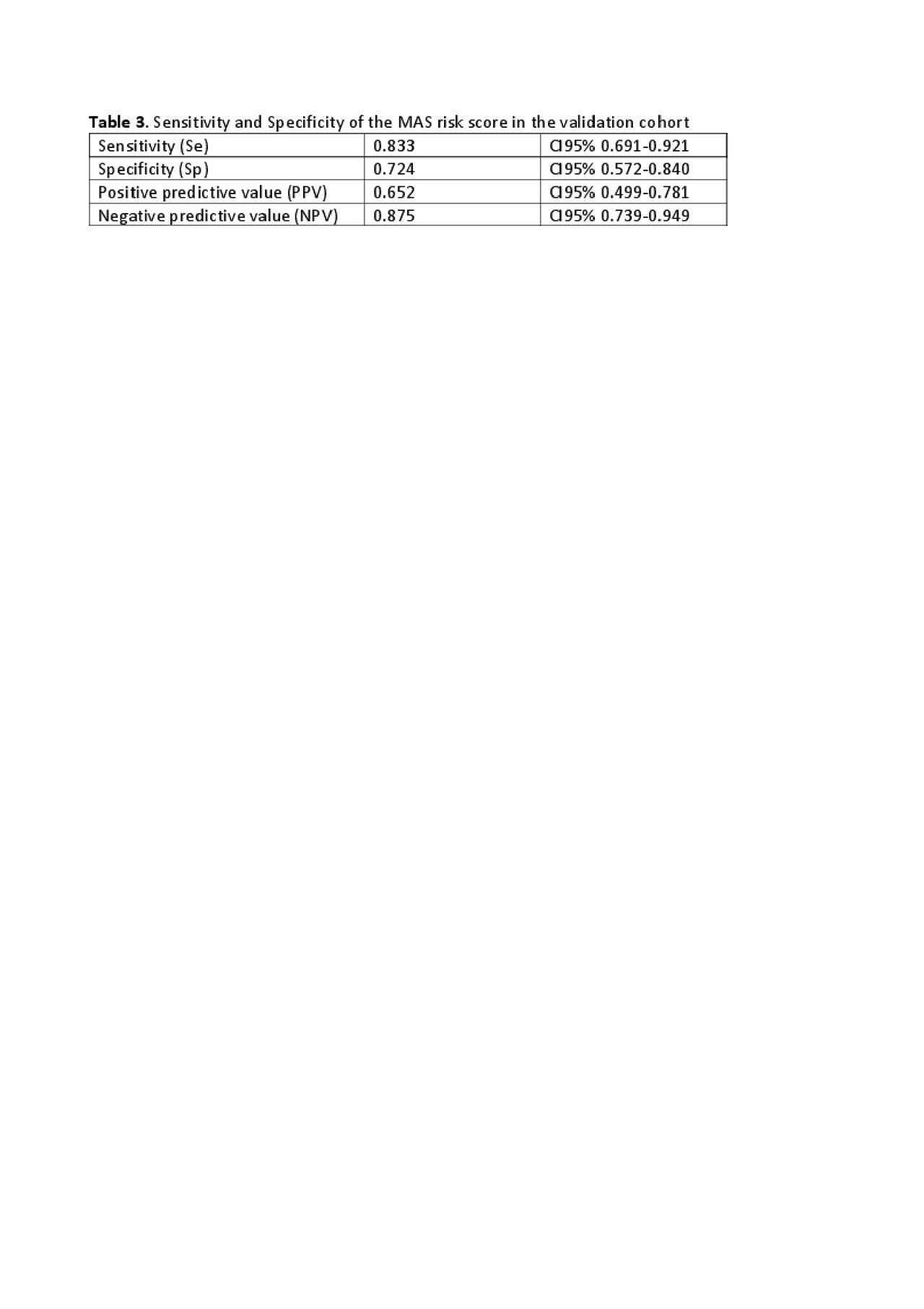
Results: Thirty-two patients, that fulfilled the 2016 classification criteria for MAS [1] at time of sampling, were excluded from the analysis. Therefore, we analysed laboratory parameters of 53 patients with sJIA, 33 of whom without history of MAS (group 1) and 20 who developed at least one episode of MAS during disease course (group 2). Levels of ferritin, AST, LDH, gGT and TGL, collected at T2, were statistically significant higher in patients with a history of MAS compared to those without a history of MAS. For each of these parameters an arbitrary cut-off was defined. In order to define the final score an arbitrary rate was attributed to each parameter (Table1). Sensitivity (Se), specificity (Sp), positive predictive value (PPV) and negative predictive value (NPV) were calculated to define the best scoring system. The scoring system with the best sensitivity was chosen (Table 2). A MAS risk score >3 identified 19 out of 20 sJIA patients with a history of MAS and 5 out of 33 sJIA patients without history of MAS. In order to validate the MAS risk score on a different population, we applied the score on 47 patients from other Paediatric Rheumatologic centres, 29 without history of MAS and 18 with at least one episode of MAS. Sensitivity and specificity of the score are reported in table 3.
Conclusion: In conclusion we developed a MAS risk score based on routine laboratory parameters, available worldwide, that can help clinicians to identify these patients early in the disease course. The initial validation analysis is promising but we need to validate the score on a larger population.
Reference
1. Ravelli A et al. Ann Rheum Dis. 2016 Mar;75(3):481-9.
To cite this abstract in AMA style:
Carbogno S, Pires Marafon D, Marucci G, Pardeo M, Insalaco A, Messia V, Sacco E, Demir F, Sozeri B, Čekada N, Jelusic M, Vougiouka O, Kostik M, Gagro A, Kessel C, Minoia F, De Benedetti F, Bracaglia C. Risk Score of Macrophage Activation Syndrome in Patients with Systemic Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/risk-score-of-macrophage-activation-syndrome-in-patients-with-systemic-juvenile-idiopathic-arthritis-2/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-score-of-macrophage-activation-syndrome-in-patients-with-systemic-juvenile-idiopathic-arthritis-2/