Session Information
Date: Tuesday, October 23, 2018
Title: 5T086 ACR Abstract: Epidemiology & Pub Health III: SLE & SSc, Big Data & Large Cohorts (2802–2807)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Previously thought to involve primarily the microvasculature, systemic sclerosis (SSc) has been increasingly linked to macrovascular disease. Cardiovascular and cerebrovascular disease are responsible for 20-30% of mortality in SSc, but few studies have shown an independent association between SSc and stroke. In this study, we assessed whether SSc was an independent risk factor for ischemic stroke.
Methods:
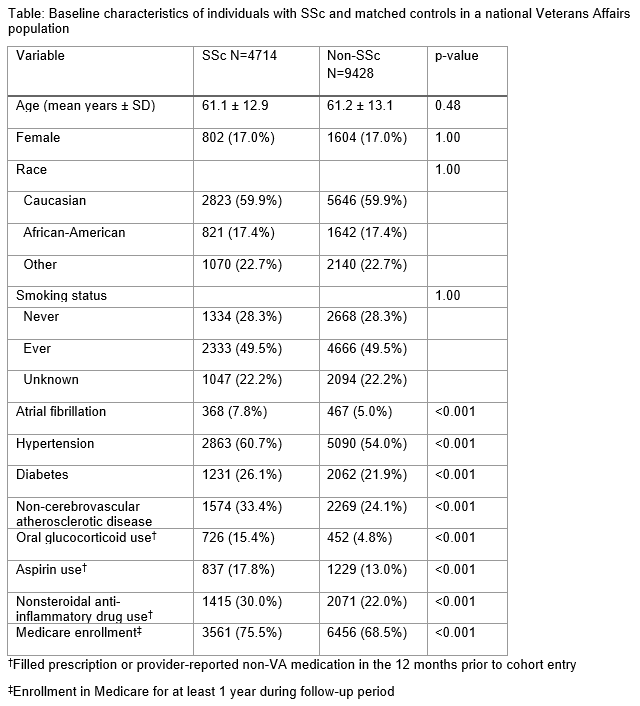
Using national VA (Veterans Affairs) electronic health record data, we conducted a retrospective cohort study comparing veterans with SSc (defined as ≥1 ICD-9 code) to a matched cohort without SSc. We matched subjects 2:1 on date of birth, sex, race, VA facility, observable time, and baseline smoking status. We collected data from October 1999 to September 2014. Follow-up began after the first ICD code for SSc (710.1) among cases, and a matched index date among controls. We excluded subjects with prior ischemic stroke. Subjects were censored after their first diagnosis of ischemic stroke, death, or last encounter, whichever came first.
Baseline comorbidities (hypertension, diabetes, atrial fibrillation, non-cerebrovascular atherosclerotic disease) were assessed prior to the index date using ICD codes. Use of oral glucocorticoids, aspirin and NSAIDs was identified by a filled prescription or provider-recorded non-VA medication in the 12 months before the index date. Medicare enrollment was used as a proxy for non-VA care, defined as enrollment for ≥1 year during follow-up. We generated a Kaplan-Meier plot to compare stroke-free survival between groups. We used an adjusted Cox regression model accounting for matching to generate hazard ratios (HRs) for ischemic stroke.
Results:
SSc patients had more cardiovascular risk factors, medication use, and Medicare enrollment (Table). Mean follow-up time was 5.1 years for SSc subjects and 5.2 years for non-SSc subjects. We found a significantly increased risk of stroke among SSc patients (12.0/1000 patient-years vs. 8.8/1000 patient-years, unadjusted HR 1.40 (95% CI 1.20 to 1.64); see Figure). After adjustment for baseline cardiovascular risk factors, medications and Medicare enrollment, the HR remained significant (1.29 (95% CI 1.09 to 1.53)).
Conclusion:
SSc is associated with a higher risk of ischemic stroke compared to non-SSc patients in the US veteran population, independent of traditional cardiovascular comorbidities and baseline medications. This is the largest study to date of cerebrovascular disease in SSc. Patients with SSc represent a population likely to benefit from targeted stroke screening or prevention therapies.
To cite this abstract in AMA style:
Ying D, Gianfrancesco M, Trupin L, Yazdany J, Greidinger E, Schmajuk G. Risk of Ischemic Stroke in Veterans with Systemic Sclerosis: A Nationwide Cohort Study [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/risk-of-ischemic-stroke-in-veterans-with-systemic-sclerosis-a-nationwide-cohort-study/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-ischemic-stroke-in-veterans-with-systemic-sclerosis-a-nationwide-cohort-study/