Session Information
Date: Monday, November 6, 2017
Title: Health Services Research Poster II: Osteoarthritis and Rheumatoid Arthritis
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
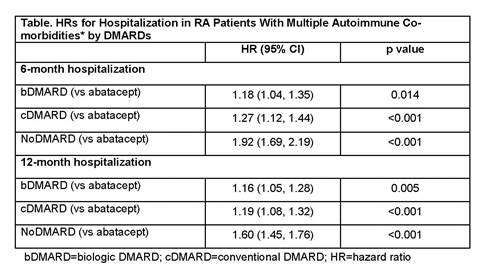
Conclusion: Among RA pts with multiple AI co-morbidities, adjusted risk of hospitalization in both bDMARD- and cDMARD-treated pts was significantly higher compared with abatacept-treated pts. Though the NoDMARD group had an even higher risk of hospitalization, this should be interpreted with caution as it comprises a heterogeneous pt population
To cite this abstract in AMA style:
Alemao E, Guo Z, Burns L. Risk of Hospitalization Among RA Patients with Multiple Autoimmune Co-Morbidities Differs By DMARD Treatment [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/risk-of-hospitalization-among-ra-patients-with-multiple-autoimmune-co-morbidities-differs-by-dmard-treatment/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-hospitalization-among-ra-patients-with-multiple-autoimmune-co-morbidities-differs-by-dmard-treatment/