Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Systemic inflammation is an independent risk factor for atherosclerosis; chronic inflammatory diseases such as systemic lupus erythematosus (SLE) are associated with increased risk of cardiovascular disease (CVD). The pathogenesis of cutaneous lupus erythematosus (CLE) is similar to SLE, with complex gene-environment interactions, autoimmunity and immune-mediated cutaneous damage. It is not known whether CLE is associated with an increased risk of CVD. Hence, we estimated the cumulative incidence of CVD in a population-based cohort of patients with CLE, and compared the risk with an age- and sex-matched cohort without CLE.
Methods: Patients with subtypes of CLE (discoid, subacute cutaneous lupus, lupus panniculitis and bullous lupus) were identified from a population-based cohort from 1965-2005. Age- and sex-matched subjects without CLE were selected from the same population. Cardiovascular events (coronary artery disease [CAD], myocardial infarction, angina, heart failure, stroke, transient ischemic attack, peripheral arterial disease) were collected via medical record review for a random sample of 66 of the 156 patients with CLE and the non-CLE subjects matched to them. The cumulative incidence of CVD was estimated using Kaplan-Meier methods. Cox models were used to estimate the relative risk of CVD in patients with CLE compared to non-CLE after adjustment for age, sex and calendar year.
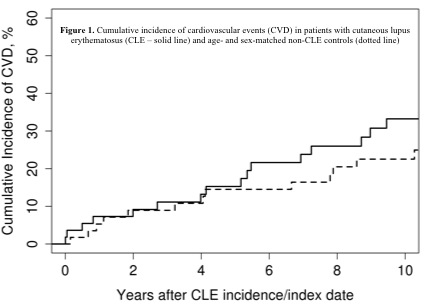
Results: We identified 66 patients with CLE (mean age at time of CLE diagnosis, 55±14y; 64% females; 68% Caucasian; mean BMI, 27.3±7.2 kg/m2; 35% current smokers), who were followed over a median follow-up of 12.0 years (interquartile range [IQR], 8.1-17.3y). Positive antinuclear antibody, anti-SSA and anti-SSB were seen in 48%, 47% and 18% of patients with CLE, respectively. Median ESR was 11 mm/hour (IQR, 4.0-25.0) and CRP 2.9 mg/dL (IQR 1.5-3.9). In this cohort, 9% were diabetic, 59% were hypertensive, 35% had hyperlipidemia and 8% had a family history of CAD; these risk factors were comparably distributed in 66 age- and sex-matched controls, except a higher prevalence of hyperlipidemia (53%, p=0.036). During follow-up, we observed 24 cardiovascular events (including 7 cases of myocardial infarction) in patients with CLE. The cumulative 1-, 5- and 10-year incidence of cardiovascular events after diagnosis of CLE was 7.3%, 15.3% and 33.2%, respectively. As compared to subjects without CLE, the risk of all cardiovascular events (hazard ratio [HR], 1.37; 95% confidence interval [CI], 0.77-2.49; p=0.29) or myocardial infarction (HR, 1.18; 95% CI, 0.77-2.49; p=0.29) was not significantly higher in patients with CLE (Figure).
Conclusion: The 10-year risk of cardiovascular events in a population-based cohort of patients with CLE is 33%. This risk is not increased as compared to age- and sex-matched non-CLE controls.
Disclosure:
A. G. Singh,
None;
C. S. Crowson,
None;
M. Davis,
None;
H. Maradit Kremers,
None;
E. L. Matteson,
None;
V. Chowdhary,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-cardiovascular-events-in-patients-with-cutaneous-lupus-erythematosus-a-population-based-study/