Session Information
Date: Sunday, November 10, 2019
Title: 3S032: Plenary I (805–809)
Session Type: Plenary Session I
Session Time: 11:00AM-12:30PM
Background/Purpose: SLE is an independent risk factor for premature cardiovascular disease (CVD) and afflicts African Americans (AA’s) 3 times more than whites. Two predominantly white cohorts have challenged the paradigm that CVD is a predominantly late complication of SLE. This study measured the risk of CVD events and predictors in a population-based incident cohort comprised mostly of AA’s over a 14-year period, starting from 2 years before diagnosis.
Methods: The Georgia Lupus Registry (GLR) is a population-based registry of SLE patients from Atlanta, Georgia. Incident SLE patients in 2002-04 met ≥4 ACR SLE criteria or 3 criteria with a final diagnosis of SLE by their board-certified rheumatologist. CVD events or CVD deaths included ischemic heart disease, cerebrovascular accident, transient ischemic attack and peripheral vascular disease as adjudicated using published guidelines. Patients were matched to the Georgia Hospital Discharge Database and National Death Index from 2000-13. CVD-related hospitalizations and deaths were classified by the first three admission or cause of death codes. Predictors of CVD events during this period were examined using Cox proportional hazards model.
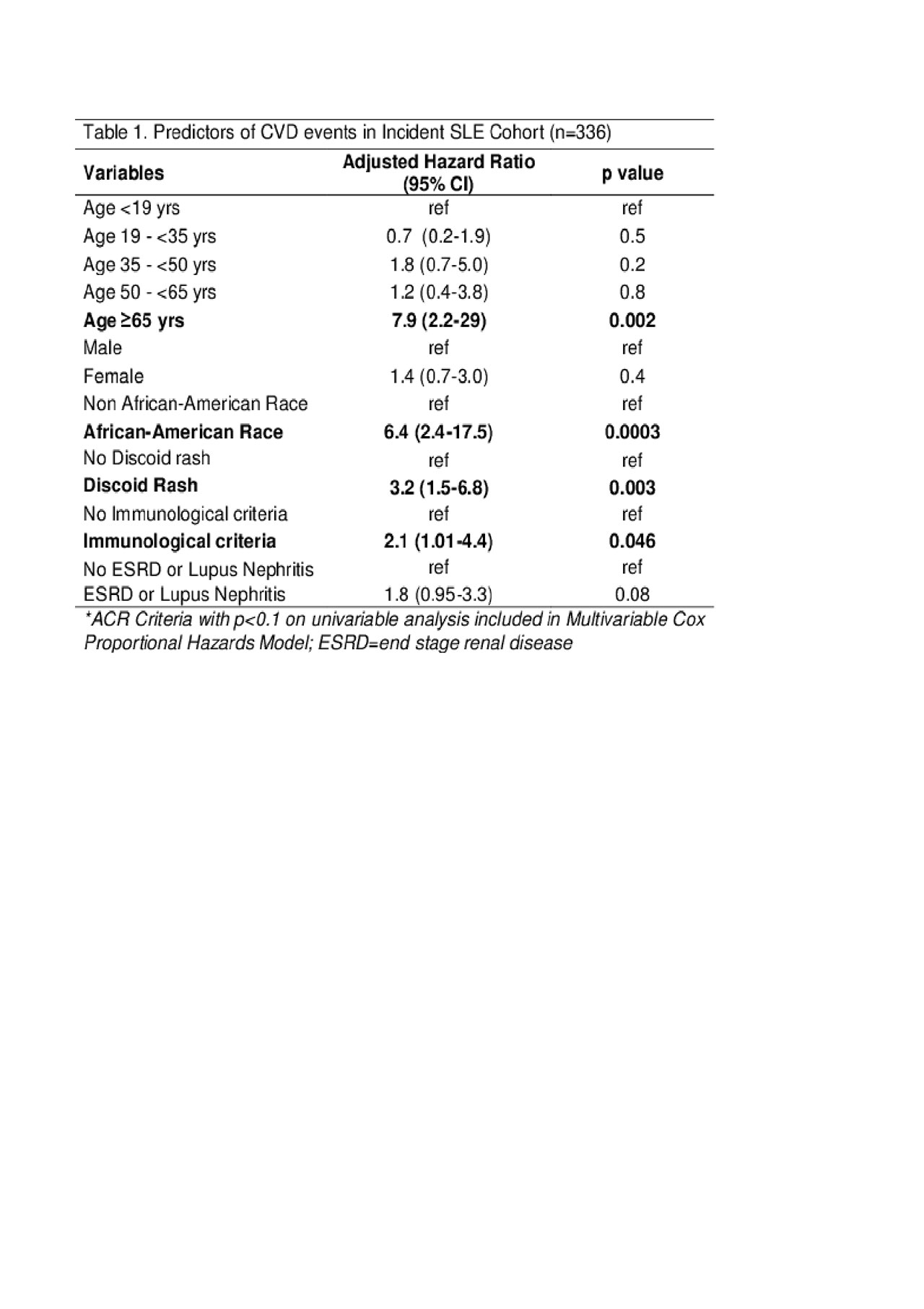
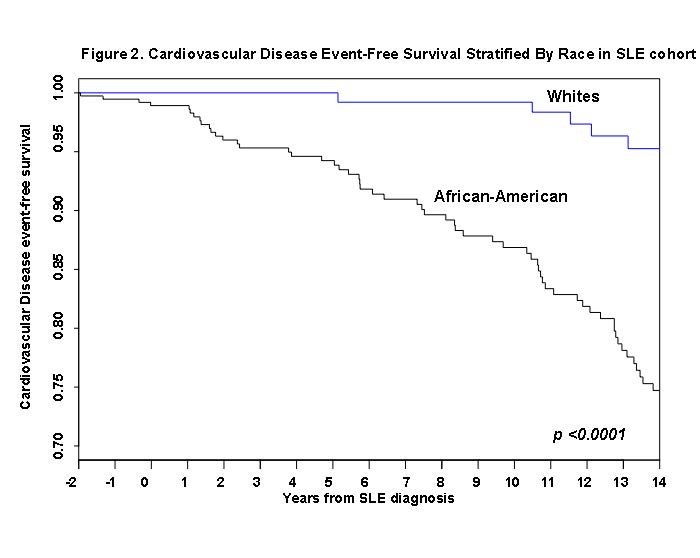
Results: Among 336 incident SLE patients, 87% were females, 75% were AA and mean age at SLE diagnosis was 40 ± 17 years. Overall, we found 31 CVD-related events and 5 CVD-related deaths from 2 years before until 10 years after SLE diagnosis and 26 CVD-related events and 1 CVD-related death from 10-14 years after SLE diagnosis. There were two CVD events which occurred >14 years after SLE diagnosis. The mean ages at SLE diagnosis and the first CVD event during 12-years of follow up starting 2 years before SLE diagnosis were 46 and 48 years, respectively, with 91% of events in females and 75% in AA. The mean ages of SLE diagnosis and first CVD event in the period 10-14 years after diagnosis were 38 and 52 years, respectively, with 70% of events in females and 76% in AA. CVD event probability is shown in Figure 1 with 22% experiencing any CVD event and the highest number of events occurring 1-2 years after SLE diagnosis. AA race predicted a 6-fold higher risk of a CVD event during the follow-up period (Adjusted HR 6.4, 95% CI 2.4-17.5; Table 1). CVD event rates in AA’s were 18-fold higher during the initial 10 years starting 2 years before SLE diagnosis (Adjusted HR 18, 95% CI 2.2-141; data not shown). Other predictors were discoid lupus (Adjusted HR 3.2, 95% CI 1.5-6.8), age >65 years (Adjusted HR 7.9, 95% CI 2.2-29), and presence of immunological criteria (Adjusted HR 2.1, 95% CI 1.01-4.4) (Table 1). The stratified Cox proportional hazard model show significantly accelerated CVD events in AA compared to whites (p< 0.0001) (Figure 2). Conclusion: We found significant CVD events peaking 1-2 years after SLE diagnosis, supporting other observations but now in a predominantly AA population-based cohort. AA race was the strongest predictor of CVD events in SLE. Future CVD prevention efforts should target such populations to reduce racial disparities, particularly around the period of SLE diagnosis.
To cite this abstract in AMA style:
Garg S, Bartels C, Drenkard C, Bao G, Lim S. Risk of Cardiovascular Disease in SLE Is Significant Early and Highlights Racial Disparities [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/risk-of-cardiovascular-disease-in-sle-is-significant-early-and-highlights-racial-disparities/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-cardiovascular-disease-in-sle-is-significant-early-and-highlights-racial-disparities/