Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The association between idiopathic inflammatory myopathies (IIMs) and malignancies in Thai population has been rarely reported. The objective of our study was to determine the risk factors of cancer in IIMs patients and to describe cancer screening methods, natural history and response to treatment in Thailand.
Methods: We retrospectively studied 74 IIMs patients according to 2017 EULAR/ACR classification criteria from 2 tertiary hospitals (Ramathibodi Hospital and Siriraj Hospital, Bangkok, Thailand). Clinical, and laboratory data, cancer screening methods, natural history, and treatment outcome were recorded. After enrollment and informed consent, blood collection for myositis-specific autoantibodies (MSAs) was done in some feasible patients to complete the laboratory data. We performed a univariate analysis using logistic regression analysis to identify clinical and laboratory predictors for cancer.
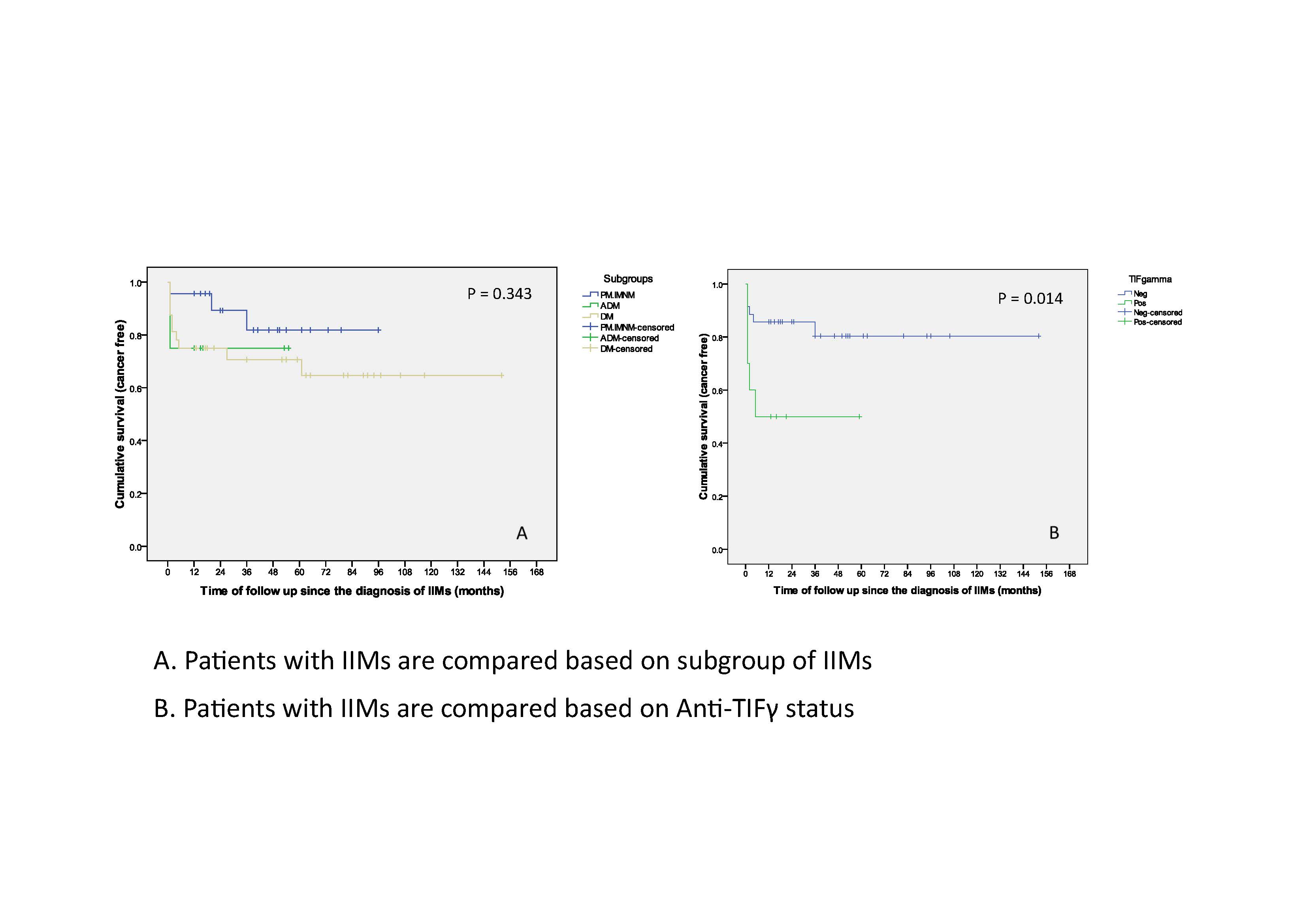
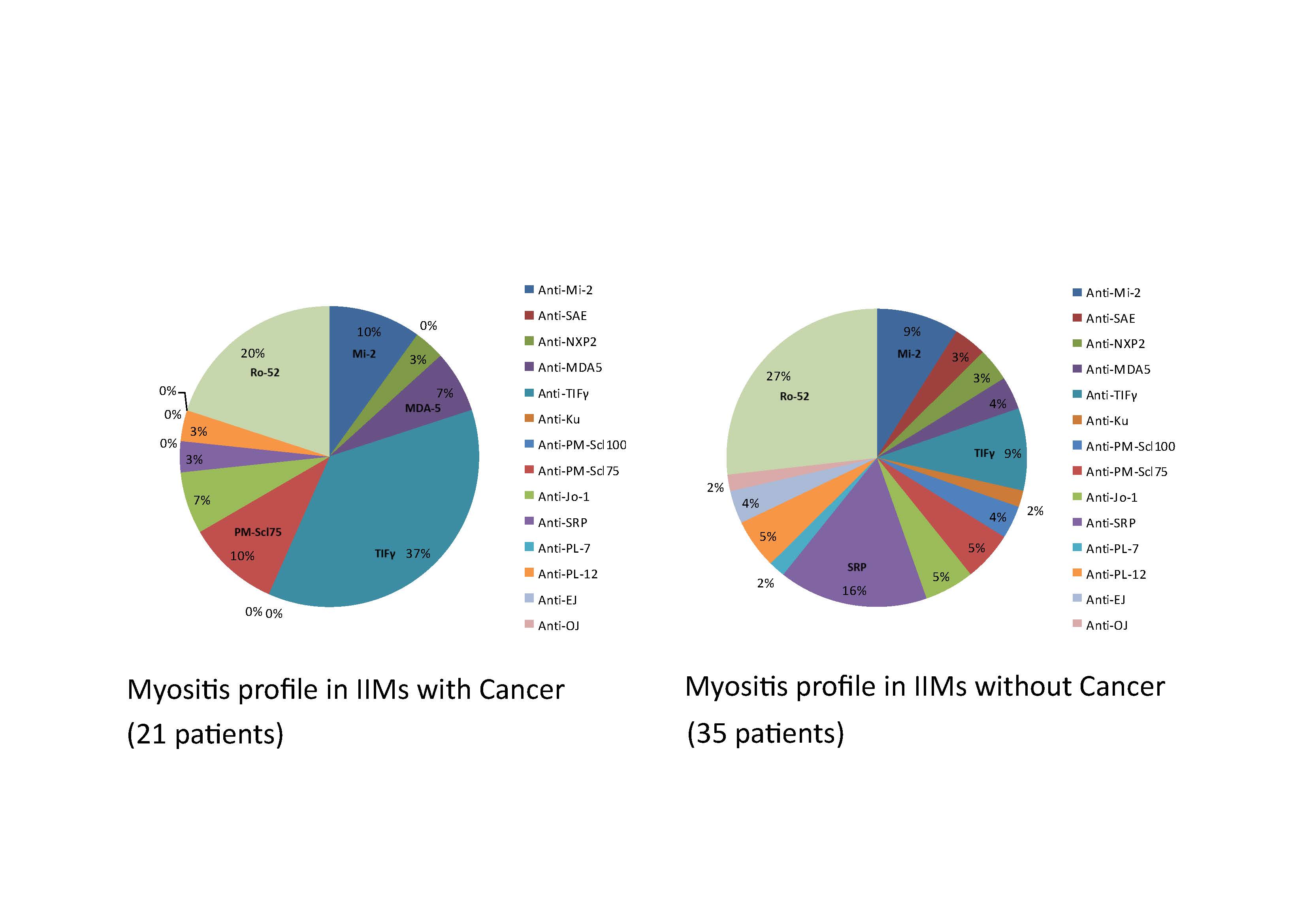
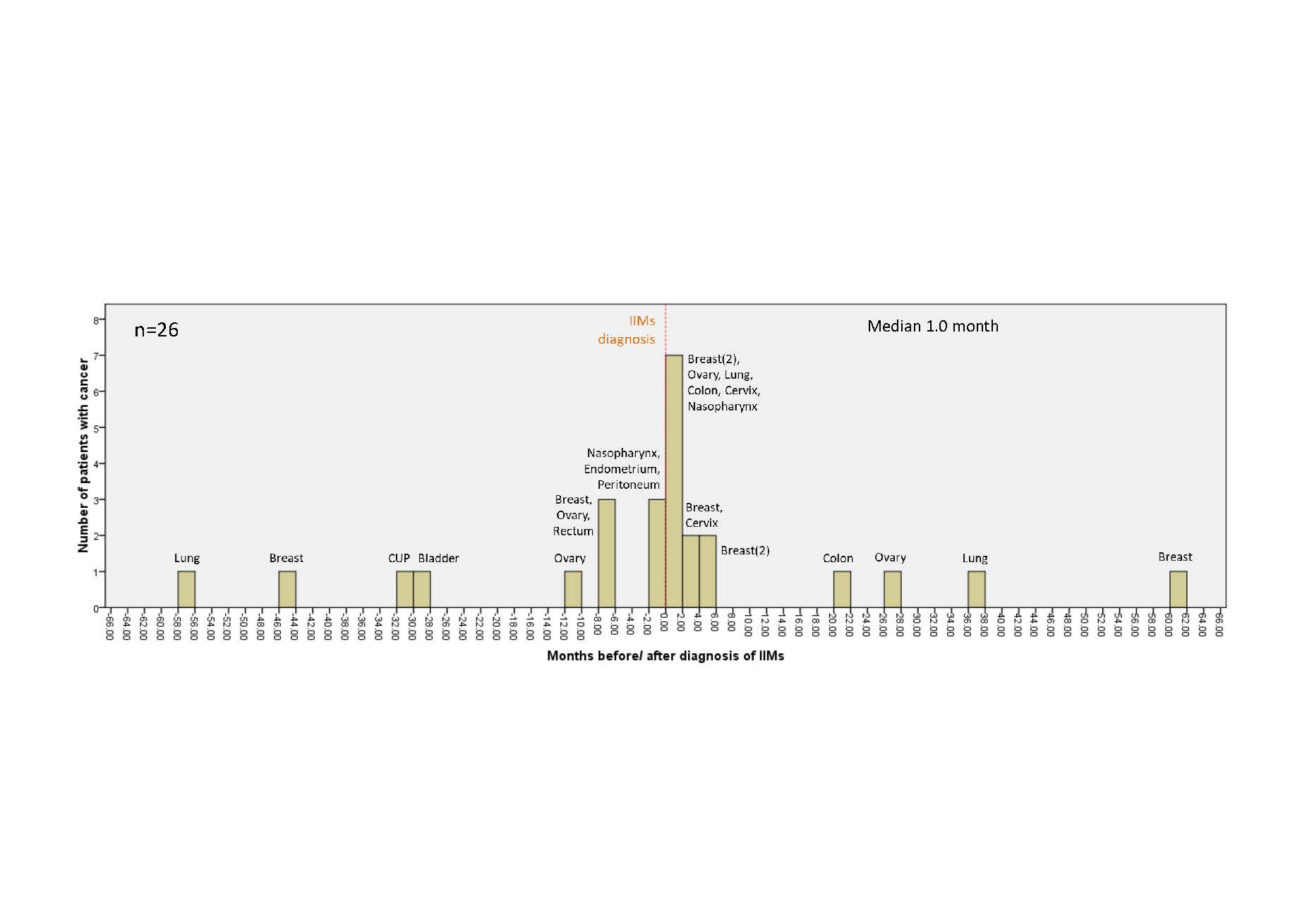
Results: Form 74 IIMs patients, we classified 25 patients in polymyositis/immune-mediated necrotizing myopathy (PM/IMNM) subgroup, 40 patients in dermatomyositis (DM) subgroup, and 9 patients in amyopathic dermatomyositis (ADM) subgroup. The mean age at diagnosis IIMs was 54.7 ± 14.7 years. Fourteen patients (18.9%) were male. Cancer was identified in 26 out of 74 IIMs patients (35.1%). Blood collection for myositis profile after enrollment was done in 17 patients. Factors that were associated with an increased risk of malignancy included DM subgroup (OR 3.27, 95%CI 1.02-10.45, P=0.045) and positive anti-TIFγ (OR 8.80, 95%CI 2.37-32.64, P=0.001). Malignancy risk also increased in IIMs patients with a positive antinuclear antibody (ANA), at titer ≥ 1:80 (OR 4.24, 95%CI 1.71-10.49, P=0.002). However, the difference was not statistically significant with the higher titer (≥1:320) of ANA (OR 1.88, 95%CI 0.63-5.59, P=0.258). While interstitial lung disease (ILD) was associated with below-than-average risk of malignancy (OR 0.11, 95%CI 0.01-0.88, P=0.040). Eighteen cases of cancer (69.2%) were diagnosed within one year before or after the diagnosis of IIMs. Median cancer diagnosis time was 1.0 month, range -57 to 61 months after IIMs diagnosis. Breast cancer was the most common cancer (31%), followed by ovarian cancer (15%). In 5 patients, cancer was detected by more extensive screening beyond age-appropriate cancer screening. IIMs patients with cancer tended to use less immunosuppressive agents compared with IIMs without cancer. However, they had a worse prognosis, with more proportion of expired patients compared to IIMs patients without cancer (OR 30.5, 95% CI = 3.45-270.83, P= 0.002). The causes of death in IIMs were cancer in 6 patients and infection in 3 patients.
Conclusion: DM subgroup and the presence of anti-TIFγ significantly increased the risk for malignancy, while ILD decreased the risk. Most cancer cases were diagnosed within one year before or after the diagnosis of IIMs, and some of them were detected by more extensive cancer screening. IIMs patients with cancer used less immunosuppressive agents, but they had a worse prognosis.
To cite this abstract in AMA style:
Pongtarakulpanit N, Yongchairat K, Kachamart W, Dejthevaporn C, Rajatanavin N, Chevaisrakul P. Risk Factors of Cancer-Associated Inflammatory Myopathies: A Multicenter Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/risk-factors-of-cancer-associated-inflammatory-myopathies-a-multicenter-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-of-cancer-associated-inflammatory-myopathies-a-multicenter-study/