Session Information
Date: Tuesday, November 14, 2023
Title: Abstracts: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: Osteoporotic fractures are the most common damage item from the Systemic Lupus Erythematosus International Collaborating Clinics (SLICC)/American College of Rheumatology (ACR) Damage Index. Previous studies reported conflicting results on risk factors for osteoporosis in systemic lupus erythematosus (SLE). The role of vitamin D in osteoporosis in the general population and in SLE remains controversial. We conducted this study to evaluate the risk factors for bone loss in SLE.
Methods: We used a longitudinal cohort that included body mass index (BMI), 25-hydroxy vitamin D levels, complement levels, SLE disease activity index (SLEDAI), and prednisone dose historically and at each visit. 4283 bone density results from 1476 different patients were abstracted from the medical record and included in the statistical analysis. We estimated the association between various patient characteristics and spinal BMD using generalized estimating equations.
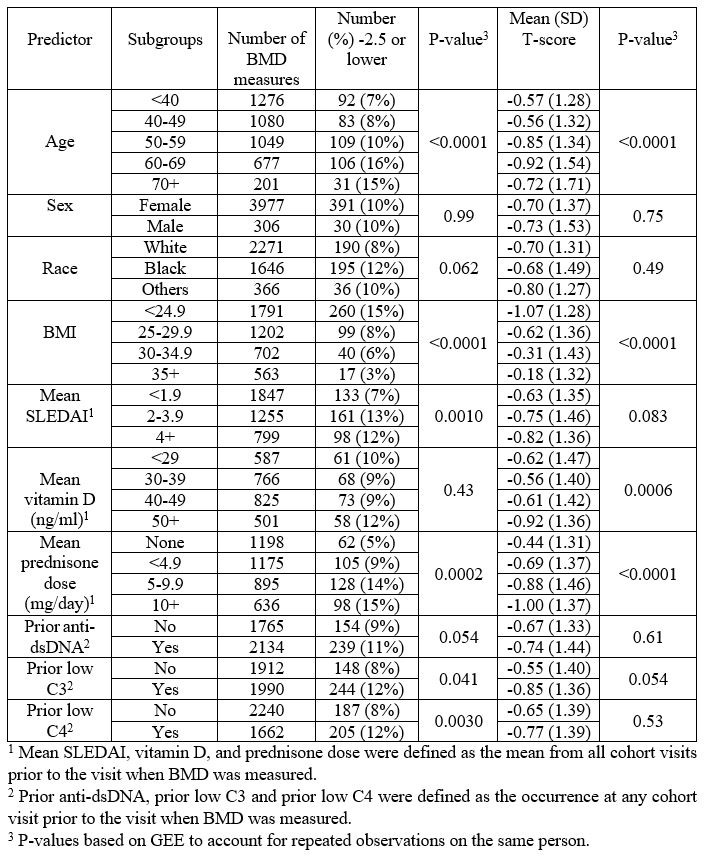
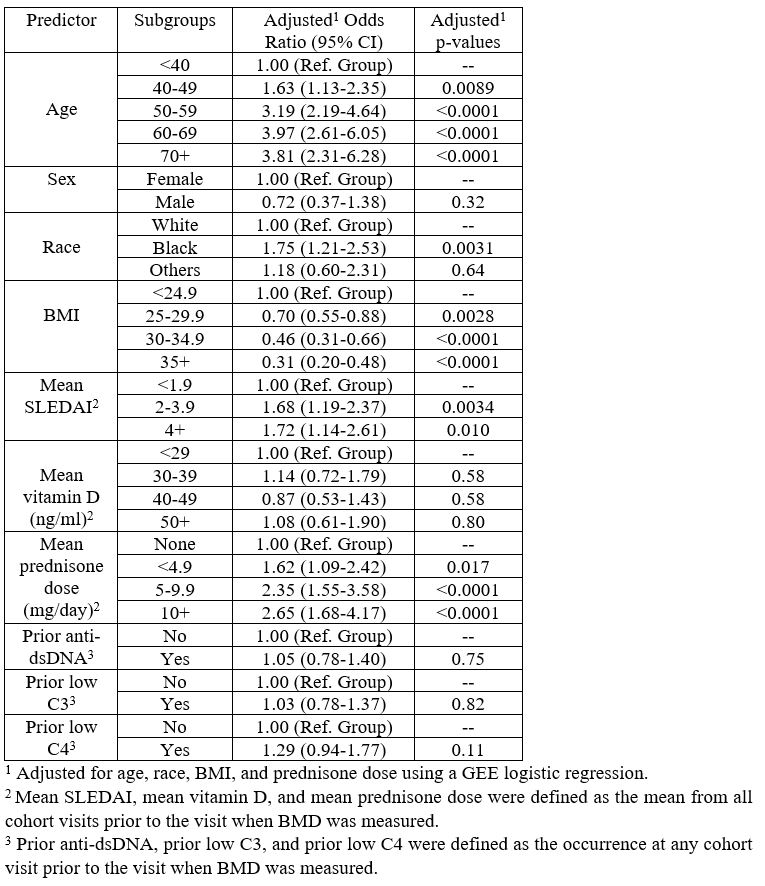
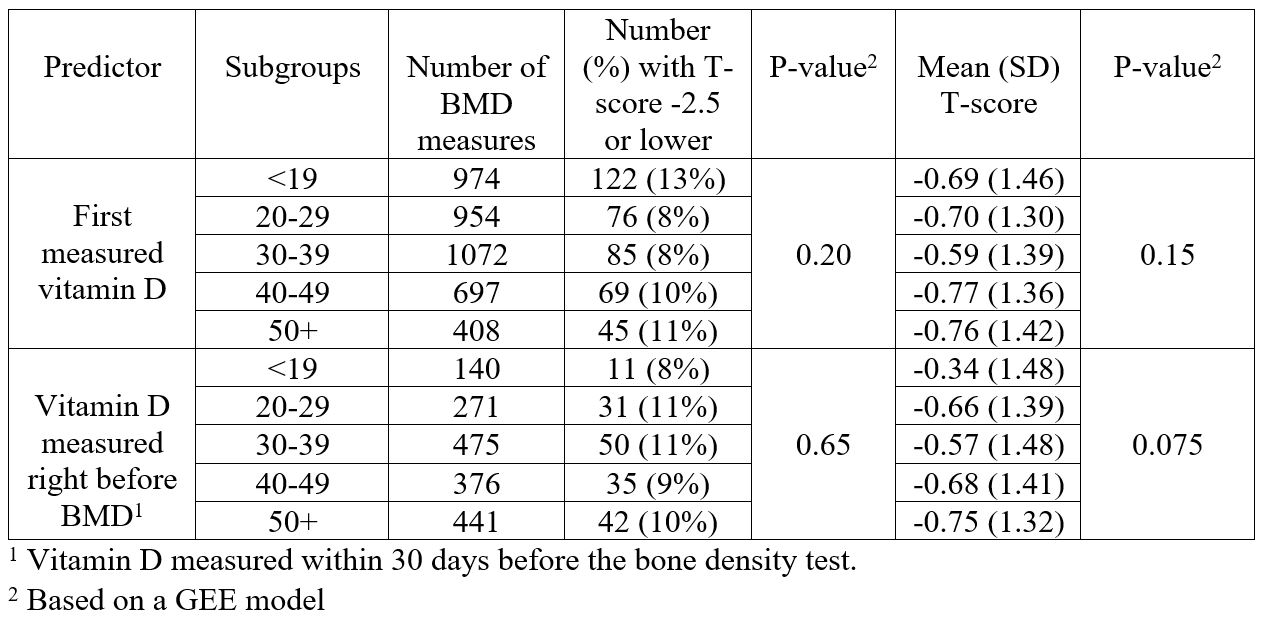
Results: A spinal T-score of -2.5 or lower was reported in 9.8% of the measurements. Univariate analysis (Table 1) showed that age, lower BMI, higher SLEDAI, mean prednisone dose, and a history of low C3 or C4 were associated with a spinal T-score of < -2.5. A multivariate analysis (Table 2) controlling for age, race, BMI, and mean prednisone dose showed higher risk of spinal osteoporosis with increasing age >40 years, Black race, mean SLEDAI >2, and history of any prednisone dose. BMI of >25 was protective. Sex, history of anti-DNA, or low C3/C4 were not associated with spinal osteoporosis in the multivariate analysis. The mean 25-hydroxy vitamin D, the first measured 25-hydroxy vitamin D, and the 25-hydroxy vitamin D level measured within 30 days prior to the bone density test were not associated with spinal osteoporosis (Table 3); but the mean 25-hydroxy vitamin D >50ng/ml was associated with lower mean spinal T-score.
Conclusion: Spinal osteoporosis in SLE was associated with age, African-American ethnicity, disease activity, and prednisone dose. Although African-Americans in the general population are protected against osteoporosis, in SLE they are at risk. Any prednisone dose – even low doses – increased osteoporosis. Vitamin D was not protective (and higher doses might have been harmful in the continuous analysis). Reduction of disease activity but without reliance on prednisone is key to osteoporosis reduction in SLE.
To cite this abstract in AMA style:
Madanchi N, Fava A, Goldman D, Magder L, Petri M. Risk Factors for Bone Loss in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/risk-factors-for-bone-loss-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-bone-loss-in-systemic-lupus-erythematosus/