Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid antibodies (aPL) are risk factors for Adverse
Pregnancy Outcome (APO). Risk stratification may include several demographic,
clinical and serological variables. Still debated is how to apply risk
stratification in the therapeutic strategy to adopt in aPL-patients during
pregnancy. Here we review the therapeutic approach to aPL-patients during
pregnancy over 30 years of experience (1985 -2015) in our center, focusing on
first-line treated pregnancies.
Methods: We collected 131 first-treated pregnancies in 131 persistently
aPL-positive women (mean age 32 years) that were prospectively followed in our
center by a multispecialistic team of Rheumatologists and Obstetricians.
Patients were classified as Primary Antiphospholipid Syndrome (PAPS) according
to Updated Sapporo criteria or as Incomplete PAPS or aPL carriers according to
their clinical history or aPL status. Patients with concomitant systemic
autoimmune diseases were excluded. aPL profile was defined as the combination
of the 3 criteria tests for aPL. APO was defined as at least one of the
followings: miscarriage (<10th week), fetal death (≥10th
week), severe preterm delivery (≤34th week) with or without
preeclampsia (PE), HELLP syndrome, and perinatal death.
Results: The type of treatment was divided in 3 main categories: combination
of low molecular weight heparin (LMWH) and low dose aspirin (LDA) (75, 57%),
monotherapy with LDA (34, 26%) and combination of corticosteroids with LDA (22,
17%; medium prednisone-dosage 76 mg/week).
We analyzed the
treatment that patients received according to clinical classification and found
that those with a diagnosis according to revised criteria (Obstetric and
Thrombotic PAPS) compared to Incomplete PAPS/aPL carriers, were more frequently
treated with combination therapy of LMWH+LDA (67% vs.39%, p:0.0025). Regarding
to serological profile, the combination therapy of LMWH+LDA was more frequently
adopted in patients with a triple positive aPL profile vs. single/double
positive ones (32% vs.3%, p:0.0001).
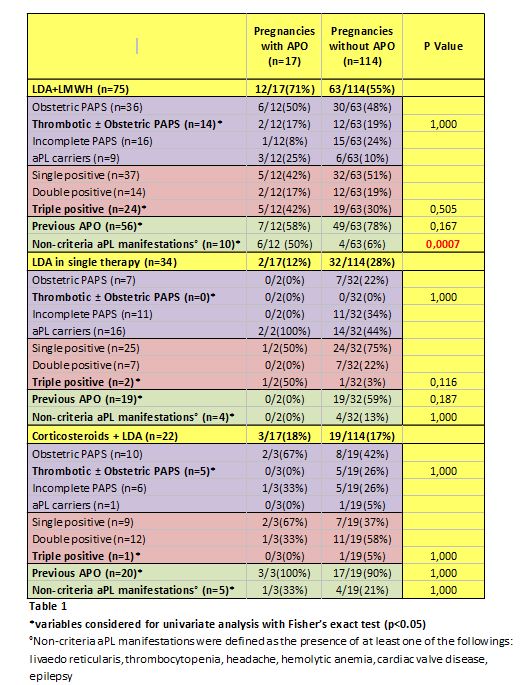
We recorded 17
APO (13%): 12 (71%) in the category of LMWH+LDA. Analyzing APO vs. non-APO
pregnancies (Table 1), we found no differences in variables that could predict
an APO (history of thrombosis, a previous APO or a triple positive aPL profile)
in any of the 3 categories . The only predicting variable for APO in the group
of LMWH+LDA was the presence of non-criteria aPL manifestations (50% vs.6%,
p:0.0007).
Conclusion: Conventional treatment comprising LMWH was preferentially given to
patients with recognized clinical and serological risk factors (definite APS
according to criteria, triple aPL positivity). The presence of non-criteria aPL
manifestations emerged as a risk factor for APO, suggesting that patients with
a more severe disease phenotype may deserve additional treatments targeting aPL
immunomodulation.
To cite this abstract in AMA style:
Lazzaroni MG, Andreoli L, Lupoli F, Aggogeri E, Bettiga E, Zatti S, Lojacono A, Ramazzotto F, Fredi M, Nalli C, Reggia R, Dall'Ara F, Taraborelli M, Gorla R, Filippini M, Taglietti M, Tincani A. Risk Factors for Adverse Pregnancy Outcome in First-Line Treated Pregnancies in Antiphospholip Antibodies-Positive Women According to Different Treatment Protocols: A Single Center Experience over 30 Years [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/risk-factors-for-adverse-pregnancy-outcome-in-first-line-treated-pregnancies-in-antiphospholip-antibodies-positive-women-according-to-different-treatment-protocols-a-single-center-experience-over-30/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-adverse-pregnancy-outcome-in-first-line-treated-pregnancies-in-antiphospholip-antibodies-positive-women-according-to-different-treatment-protocols-a-single-center-experience-over-30/