Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with Systemic Lupus Erythematous (SLE) and Rheumatoid Arthritis (RA) had profound negative effects on their health-related quality of life (HRQoL) that can be assessed using the 36 item Medical Outcome Study Short-Form survey (SF-36). Remission might have a different impact on patient´s HRQoL depending on the specific disease diagnosis.
In 2004 and 1999, respectively, recent-onset rheumatoid arthritis (RA) and systemic lupus erythematous (SLE) cohorts were initiated; the 36 item Medical Outcome Study Short-Form survey (SF-36) was incorporated to routine assessments from 2005 onwards in the SLE cohort and the SF-36v2 beginning from enrollment in the RA cohort. Objectives of the study were to compare the SF-36v2 scores between patients from both cohorts who achieved sustained remission (SR) and to define the role of disease diagnosis as associated to SF-36v2 normative data.
Methods: SLE and RA were diagnosed based on corresponding ACR classification criteria. Routine assessments were performed every 2-6 months and included at least the SLE disease activity index 2000 update (SLEDAI-2K) for SLE patients, and the Disease Activity Score (28 joints) (DAS28) for RA patients.
SR was considered when RA and SLE patients achieved at least 12 months of continuous follow-up with either SLEDAI-2K=0 or DAS28 ≤2.4, respectively. Up to December 2015, data from 172 RA patients and 211 SLE patients respectively, were reviewed.
SF-36v2 scores were available for the totality of SR assessments. The SF-36v2 licensee performed the re-scoring of the SF-36 that was used in the SLE cohort. In all the cases, Spanish (for México) versions were used and scoring was adjusted by gender and age. Logistic regression models were used to investigate factors associated with normative SF-36v2. Written informed consent was obtained from all patients.
Results: A higher proportion of RA patients achieved SR: 106 (58%) RA patients vs. 75 (30.6%) SLE patients, p≤0.001. SR was achieved earlier in patients from the former group: (mean±SD) follow-up was 30.8±23.9 months vs. 59.4±37.5 months in SLE patients, p≤0.001. The length of time in SR and the number of patients who had a disease flare were similar in both cohorts.
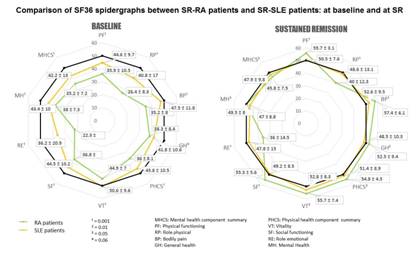
At baseline, RA patients scored significantly lower all the domains of the SF-36v2 and both the mental and physical summary measures, than SLE patients. At SR, RA patients scored better than SLE patients in 6 out of 8 domains of the SF-36v2 and the physical health component summary (Figure).
Age (ß: 1.06, 95% CI: 1.02-1.1, p=0.03) and SLE diagnosis (ß: 9.64, 95% CI: 3.61-25.75, p≤0.001) were predictors of not achieving normative physical component summary measure.
Conclusion: Patient´s perspective of (absence of) disease activity represents an important aspect of the assessment of rheumatic diseases. RA patients in SR achieved better quality of life than SLE patients.
Figure.
To cite this abstract in AMA style:
Pascual-Ramos V, Contreras-Yáñez I, Valencia-Quiñones K, Romero-Diaz J. Rheumatoid Arthritis Patients Achieved Better Quality of Life Than Systemic Lupus Erythematosus Patients at Sustained Remission: The Impact of Disease Diagnosis on Health-Related Quality of Life Outcomes [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/rheumatoid-arthritis-patients-achieved-better-quality-of-life-than-systemic-lupus-erythematosus-patients-at-sustained-remission-the-impact-of-disease-diagnosis-on-health-related-quality-of-life-outco/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatoid-arthritis-patients-achieved-better-quality-of-life-than-systemic-lupus-erythematosus-patients-at-sustained-remission-the-impact-of-disease-diagnosis-on-health-related-quality-of-life-outco/