Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Methotrexate (MTX) and mycophenolate (MMF) are two common medications for both lupus (SLE) and rheumatoid arthritis (RA). Both medications are contraindicated in pregnancy, necessitating counseling regarding family planning and contraceptive adherence. The ACR recommends that contraceptive counseling and pregnancy planning be conducted regularly for all patients with rheumatologic diseases (Sammaritano et. al. 2020). Observational studies demonstrate low frequency of pregnancy and contraceptive counseling in patients with rheumatologic disease (Yazdany et. al. 2010; Ingram et. al. 2021).
Methods: We conducted a retrospective cohort study identifying female patients, between the ages of 18 and 45, with a diagnosis of SLE or RA using ICD-9 and ICD-10 codes. We reviewed patient charts to determine whether MMF or MTX had been prescribed. We recorded whether pregnancy counseling or contraception documentation occurred at the index visit or during any visits while on these medications. We extracted contraceptive methods, and demographic data including age, language, and insurance status.
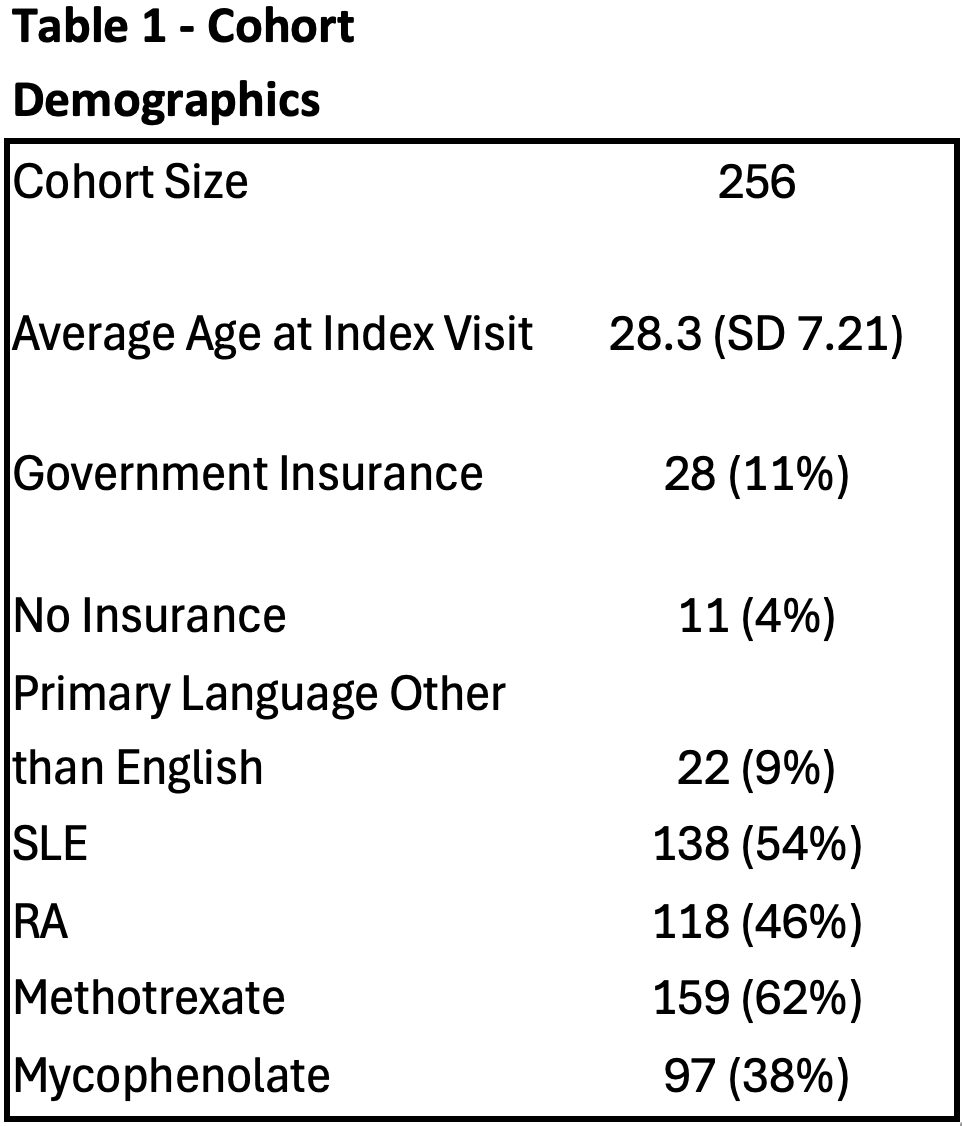
Results: In our cohort of 256 patients (SLE: N = 138, 54%; RA: N = 118, 46%, Table 1), the average age was 28. 159 patients were taking MTX (62%) and 97 patients were taking MMF (38%). The most popular types of contraception included contraceptive pills (34%), IUD (22%), and barrier methods (10%).
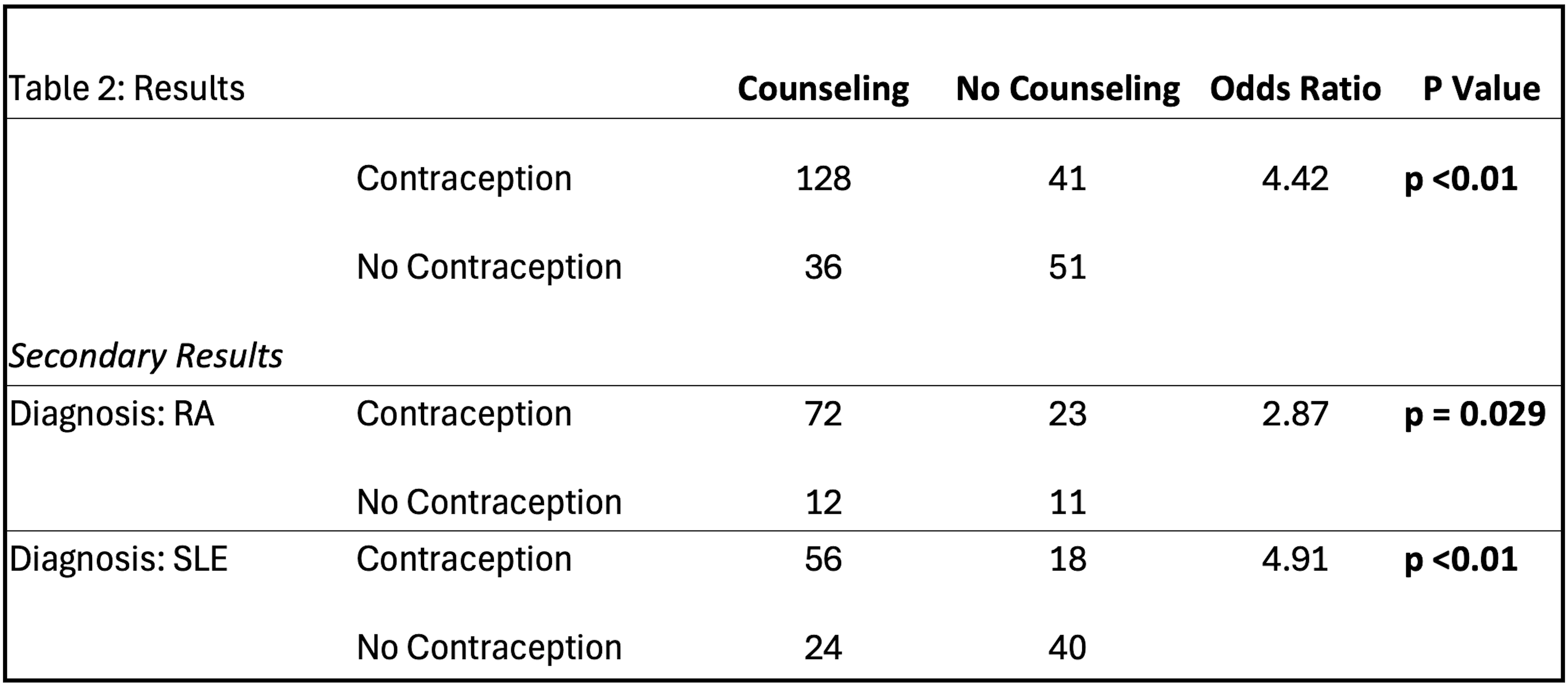
Of the 256 patients, 164 patients (64%) were counseled, and 169 patients (66%) were documented to adhere to contraception. Counseling was documented in 81% of patients with RA and 54% of patients with SLE. There was a significant association between documentation of contraception counseling and contraception adherence in the total cohort (OR= 4.42, p < 0.01). This was true for patients with SLE and RA (SLE OR = 4.91, p< 0.01; RA OR 2.87, p = 0.029, Table 2). Patients were more likely to be counseled when the medication was started in the outpatient setting (OR = 7.24; p = 0.003), but primary language and insurance status were not associated with a difference in counseling incidence.
There was a statistically significant difference in both counseling and contraception documentation between patients with RA and SLE, with patients with RA being more likely to receive counseling (p < 0.01) and document contraception use (p = 0.024).
Conclusion: Documentation of contraception counseling was associated with a four-fold increase in the likelihood of contraception adherence. A reproductive care gap exists in patients with SLE and RA who take teratogenic medications. Future studies should aim to identify and remove barriers to contraceptive counseling and adherence, especially for patients with significant co-morbidities and medical complexity.
References:
Ingram, E., et al. Contraceptive Use in Women of Childbearing Ability With RA. J. Clin. Rheumatol. (2021)
Sammaritano, L. et al. 2020 ACR Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases. Arthritis Care Res. (2020)
Yazdany, J. et al. Contraceptive counseling and use among women with SLE: a gap in health care quality? Arthritis Care Res. (2011)
To cite this abstract in AMA style:
Kompa K, Kyttaris V. Rheum for Improvement: Contraception Counseling and Adherence in Patients with Lupus and Rheumatoid Arthritis on Teratogenic Medications [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/rheum-for-improvement-contraception-counseling-and-adherence-in-patients-with-lupus-and-rheumatoid-arthritis-on-teratogenic-medications/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheum-for-improvement-contraception-counseling-and-adherence-in-patients-with-lupus-and-rheumatoid-arthritis-on-teratogenic-medications/