Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Gaps in systemic lupus (SLE) care are believed to contribute to higher kidney failure (ESKD), acute care use, mortality, and disease damage in US patients who are Black or disadvantaged. Such disparities in HIV declined >20% by addressing key care steps. We hypothesized that, SLE retention in care by visits or labs would differ by neighborhood disadvantage. We also examined how gaps in SLE care associate with ESKD, acute care, or death to inform actions to reduce disparities.
Methods: This cohort study used a 20% US Medicare sample of patients ≥18 yrs with >12 mos of Medicare A-B in 2013-14 (subset: Part D). SLE was identified by validated criteria: 1 SLE hospital code, 1 rheumatologist code, or 2+ SLE codes 2 mos apart. Baseline comorbidity was measured 6 mos prior. Over 6 mos, 4 care steps were examined: 1) visit retention: ≥ 1 rheumatology visit; 2) lab retention: a C3, C4 or a double-stranded DNA test (two if nephritis); 3) HCQ use: any HCQ claim; and 4) HCQ adherence: >80% of days covered. Outcomes included acute care (emergency or hospital visits) or death, ESKD or death followed until end of data, 12/31/2014. We assessed for disparities by racial identity and neighborhood disadvantage area deprivation index (ADI) quintile. Cox proportional hazards models were used to report hazards ratios (HR) and 95% confidence intervals (CI) for 2 outcomes by 4 care steps controlling for covariates.
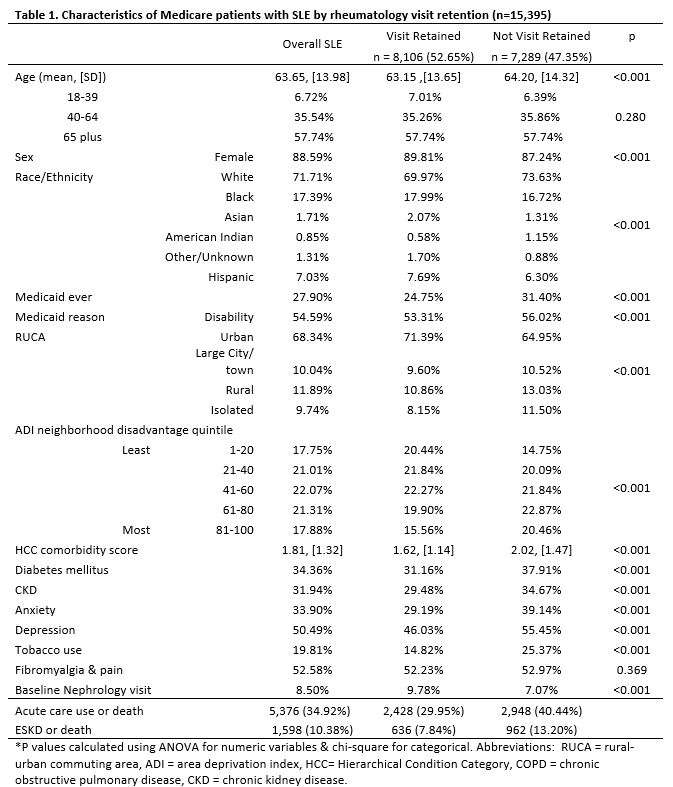
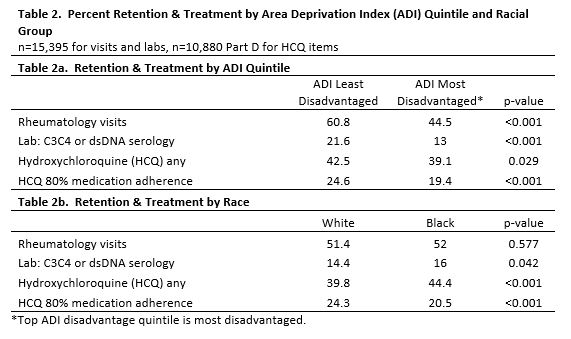
Results: Among 15,395 patients with SLE, 88.6% were female and 17.4% identified as Black (Table 1). Overall, 27.9% had prior Medicaid; 35.2% of Black identifying patients lived in the most disadvantaged ADI quintile neighborhoods. Patients living in high ADI (more disadvantage) had 16% lower visit retention (44.5% vs 60.8%, p< 0.001 Table 2), lower lab retention (13% vs 26.6%, p< 0.001), received less HCQ (39.1 vs 42.5%, p=0.029), and 5.2% lower HCQ adherence (19.4% vs 24.6%, < 0.001) than less disadvantaged neighborhoods. Black patients experienced slightly more visit retention (52% vs 51.4%, p=0.577), lab retention (16% vs 14.4%, p=0.042), and more HCQ use (44.4% vs 39.8%, p< 0.001), but lower HCQ adherence (20.5% vs 24.3%, p< 0.001) than White patients.
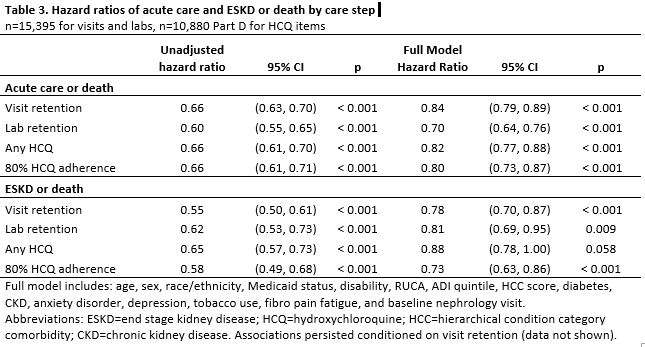
Overall, 34.9% received acute care or died over 1 year; rates were 10.5% higher without visit retention (Table 1). 10.4% experienced ESKD or death; rates were 5.4% higher without visit retention. Adjusted Cox models showed that all care retention steps predicted lower acute care or death (HR 0.70-0.84, all p< 0.001, Table 3) and most retention steps predicted lower ESKD or death (HR 0.73-0.81, all p< 0.05, except any HCQ, p=0.058). Lab retention associated most with reduced acute care/death HR 0.70 (0.64, 0.76); HCQ adherence most strongly associated with lower ESKD/death, HR 0.73 (0.63, 0.86).
Conclusion: Lupus outcomes correlated with lupus visits and labs, with strongest associations between SLE labs and acute care-free survival. HCQ 80% adherence most strongly correlated with ESKD-free survival. Care varied more by ADI than race alone, supporting ADI use in ACR quality reporting, and a need for new care strategies to advance health equity using a social determinants lens to improve SLE outcomes.
To cite this abstract in AMA style:
Bartels C, Yu A, Elwert F, Gilmore-Bykovskyi A, Powell W, Garg S, Kind A. Retention in Rheumatology Care and on Hydroxychloroquine and SLE Outcomes by Neighborhood Disadvantage: A Medicare Cohort Study of Acute Care and Kidney Failure [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/retention-in-rheumatology-care-and-on-hydroxychloroquine-and-sle-outcomes-by-neighborhood-disadvantage-a-medicare-cohort-study-of-acute-care-and-kidney-failure/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/retention-in-rheumatology-care-and-on-hydroxychloroquine-and-sle-outcomes-by-neighborhood-disadvantage-a-medicare-cohort-study-of-acute-care-and-kidney-failure/