Session Information
Date: Sunday, November 7, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Manifestations (0855–0896)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Despite weight-based dosing, hydroxychloroquine (HCQ) efficacy varies between individuals. Our meta-analysis based on several studies found that low HCQ levels increased risk of lupus flare, while high levels increased the risk of macular toxicity. Aside from body weight, factors influencing HCQ levels are not well defined. Understanding such factors could guide clinicians to adjust HCQ doses, with the aim of controlling lupus disease activity while minimizing toxicity. Thus, we examined individual factors associated with variations in HCQ levels. We also evaluated the impact of HCQ levels on SLE disease outcomes.
Methods: Inclusion criteria were: a) age ≥18 years, b) 1997-ACR, 2012-SLICC or 2019-ACR/EULAR confirmed SLE, c) prescribed HCQ ≥1 month before enrollment. We measured consented patients’ whole blood HCQ levels after clinic visits. We abstracted data on patients’ demographics, disease characteristics, laboratory values, SLE disease activity index (SLEDAI), and patient-reported adherence (0-100% MASRI Visual analogue scale (VAS); ≥80% adherence) on the day of the visit. We measured HCQ blood levels by liquid chromatography mass spectrometry. We used linear and logistic regression models to test associations between interindividual factors and HCQ blood levels, and between HCQ levels and SLE outcomes.
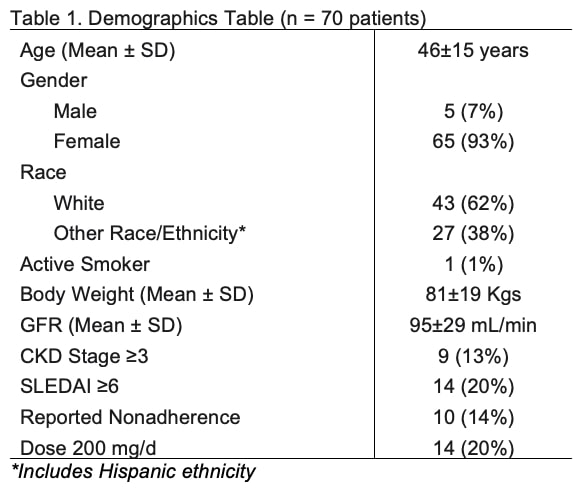
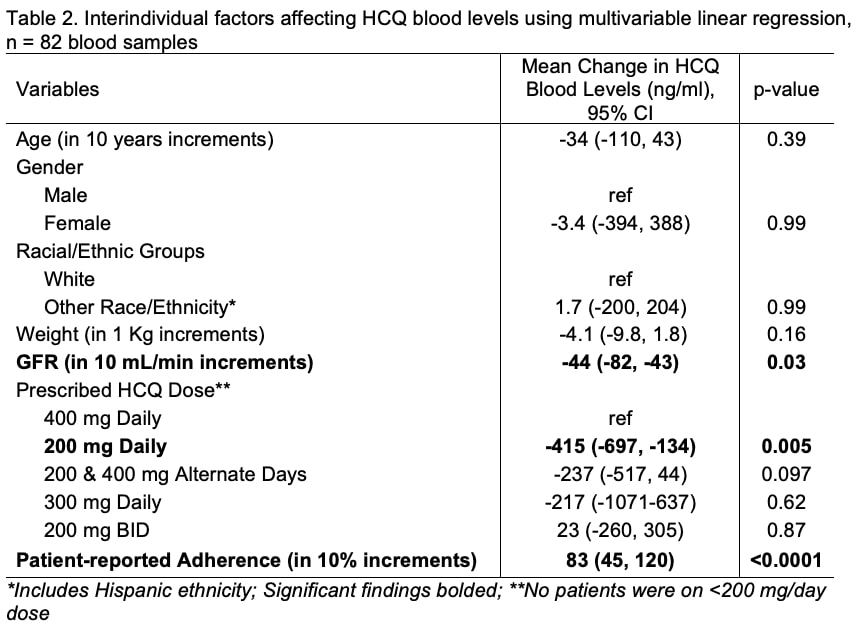
Results: Patient and clinical characteristics are summarized in Table 1. Among 82 samples collected from 70 patients between 8/1/20 and 5/20/21, mean±SD HCQ levels were 813±502 ng/ml. HCQ dosing, renal function and adherence were the key variables predicting HCQ levels. We noted that regardless of adjustment for body weight, patients taking 200 mg/day had lower HCQ levels (Mean Difference -415 ng/ml, CI -134, -697; p 0.005, Table 2). We found an inverse relationship between renal function and HCQ blood levels. For every 10 mL/min increment in glomerular filtration rate (GFR), there was a 44 ng/mL decline in HCQ levels (CI -43, -84; p 0.03). Further, we found that patients with CKD stage ≥3 had significantly higher HCQ levels by 345 ng/ml (CI 42, 648; p 0.02, data not shown). Finally, we found that every 10% increase in patient-reported adherence predicted an 83 ng/ml increase in HCQ levels (CI 45, 120; p < 0.001). We found no associations between weight and HCQ levels.
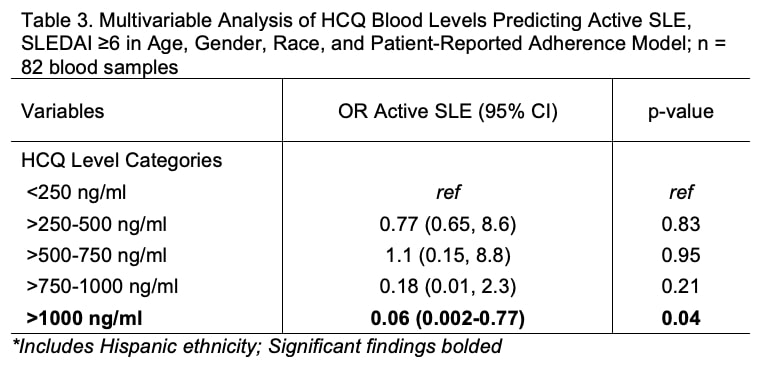
HCQ levels ≥500 ng/ml predicted 40-fold higher odds of patient-reported adherence by VAS (p 0.0007, data not shown). There was a good correlation between HCQ levels and patient-reported adherence (0.55, p < 0.001, data not shown). Finally, we noted that HCQ levels ≥1000 ng/ml predicted 94% lower odds of active SLE (SLEDAI ≥6) (OR 0.06, CI 0.002-0.77, p 0.039, Table 3) and clinically meaningful change in SLEDAI (-2.7, CI -1.1, -4.4, p 0.036).
Conclusion: We found that HCQ dose, adherence and renal function predicted significant variations in HCQ blood levels. Patients with CKD stage ≥3 had markedly higher HCQ levels, which could portend higher HCQ toxicity in this group. Conversely, prescribing lower HCQ doses could permit higher flare risk. Our findings support that individualizing HCQ dosing based on GFR could benefit SLE patients. Future work will focus on how to effectively individualize dosing to reduce toxicity and flares in diverse SLE patients.
To cite this abstract in AMA style:
Garg S, Hansen K, Chewning B, Bartels C. Renal Function, Adherence and Low Hydroxychloroquine Dosing Predict HCQ Blood Levels and Lupus Disease Activity [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/renal-function-adherence-and-low-hydroxychloroquine-dosing-predict-hcq-blood-levels-and-lupus-disease-activity/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-function-adherence-and-low-hydroxychloroquine-dosing-predict-hcq-blood-levels-and-lupus-disease-activity/