Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: Fibromyalgia (FM) is a widely recognized and commonly diagnosed disorder that has also been the subject of thousands of research studies. There is no gold standard definition of FM, but well-vetted diagnostic criteria exist. The extent to which these criteria are used for diagnosis by community physicians is uncertain. In 3 large epidemiologic studies, we compared physician diagnosis with diagnosis by published criteria to determine the level of agreement between criteria and physician diagnosis. We also compared different research criteria in clinical settings to obtain estimates of agreement among competing FM criteria
Methods: We compared 4 sets of published FM diagnostic criteria: The 2016 modification of ACR 2010 criteria (FM 2016), ACTTION-APS Pain Taxonomy criteria (AAPT), London widespread pain criteria (LFESSQ 4), and London widespread pain plus fatigue abnormality (LFESSQ 6) in 4,348 patients using Forward, the National Data Bank for Rheumatic Diseases (NDB) as to agreement with FM 2016. We then compared reported physician (MD) diagnosis of FM with FM 2016 criteria in 3,276 consecutive primary care patients (PC), 2531 persons in a German general population survey (GPS), and 8486 in the US National Health Interview Survey (NHIS). We used Cohen’s kappa and the Phi coefficient as measures of agreement, and the polysymptomatic distress (PSD) scale as a measure of FM symptom severity.
Results: As shown in Table 1, FM 2016, LFESSQ 6 and AAPT criteria tapped into similar concepts, yielding kappa and phi coefficients of .726-.752, prevalence values between 21.4-30.1%, and PSD scores between 16.4-20.9. Figure 1 shows increased cases meeting AAPT criteria compared with FM 2016. None of the physician criteria adequately agreed with FM 2016 criteria (all kappa and phi statistics < .300). As shown in Figure 2, many patients who were MD diagnosis positive clearly failed FM 2016 criteria, and many MD classification negative subjects satisfied FM 2016 criteria. The lower the kappa and phi values the less severe were values of PSD (9.6-12.4) among MD diagnosed patients.
Conclusion: Diagnosis by formal criteria had conceptually adequate agreement overall, but at the patient level 34% of positive diagnoses disagreed between FM 2016 and AAPT. Physician diagnosis and formal criteria are in poor agreement. As shown in Figure 2, this is not merely failure to diagnose, but represents incorrect classification. There is not “one” FM. Diagnoses based on physician diagnoses (not formal criteria), such as in hospital and insurance company registries have limited validity and reliability, and kappa and phi values so low as to render diagnosis almost meaningless. FM is a symptom severity-based diagnosis, but until FM care and research rely primarily on reliable continuous severity scales, FM will remain an uncertain diagnosis. Some of the disagreement between MD diagnosis and FM criteria may represent changes in severity over time that are not captured in our data, but also raise the question of the nature of the FM diagnosis.
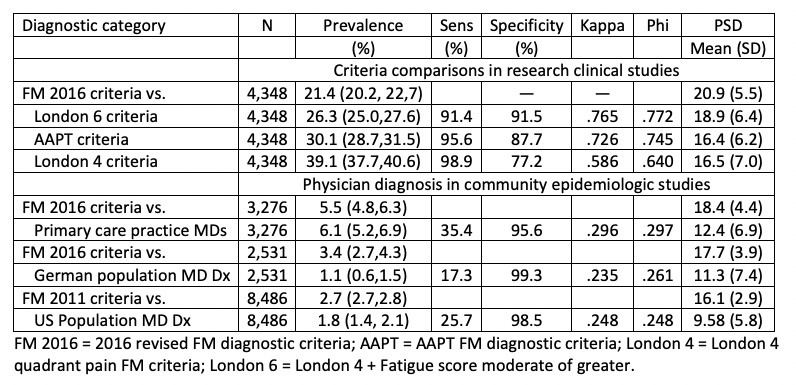 Table 1. Characteristics and agreement according to FM diagnostic methods.
Table 1. Characteristics and agreement according to FM diagnostic methods.
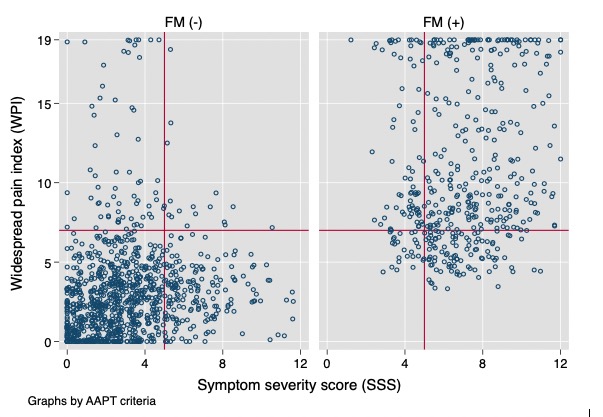 Figure 1. Plot of symptom severity score (SSS) against widespread pain index (WPI) according to AAPT criteria status. Horizontal line at 7 is level of WPI required by FM 2016 criteria. A small amount of random noise is added to each observation so that observations are seen more clearly. Vertical line at 5 is level required by FM 2016 criteria.
Figure 1. Plot of symptom severity score (SSS) against widespread pain index (WPI) according to AAPT criteria status. Horizontal line at 7 is level of WPI required by FM 2016 criteria. A small amount of random noise is added to each observation so that observations are seen more clearly. Vertical line at 5 is level required by FM 2016 criteria.
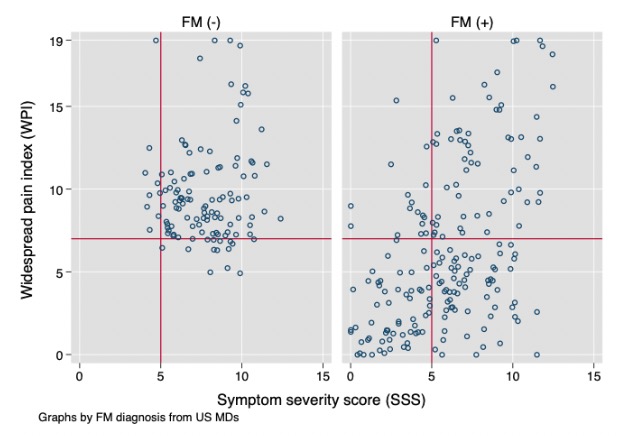 Figure 2. Plot of symptom severity score (SSS) against widespread pain index (WPI) according to reported US primary care physician diagnosis. Horizontal line at 7 is level of WPI required by FM 2016 criteria. Vertical line at 5 is level required by FM 2016 criteria. A small amount of random noise is added to each observation so that observations are seen more clearly. Data include only patients who are FM positive by FM2016 or ad hoc US primary care physician criteria.
Figure 2. Plot of symptom severity score (SSS) against widespread pain index (WPI) according to reported US primary care physician diagnosis. Horizontal line at 7 is level of WPI required by FM 2016 criteria. Vertical line at 5 is level required by FM 2016 criteria. A small amount of random noise is added to each observation so that observations are seen more clearly. Data include only patients who are FM positive by FM2016 or ad hoc US primary care physician criteria.
To cite this abstract in AMA style:
Wolfe F, Rasker J, Walitt B. Reliability and Validity Issues in Fibromyalgia Diagnosis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/reliability-and-validity-issues-in-fibromyalgia-diagnosis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/reliability-and-validity-issues-in-fibromyalgia-diagnosis/
