Session Information
Date: Sunday, November 13, 2016
Title: Imaging of Rheumatic Diseases I: Advanced Imaging in RA and Spondyloarthritides
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Tenosynovitis in the hand occurs frequently and early in rheumatoid arthritis (RA) and sensitive outcome measures are important to assess and monitor the inflammatory activity. Magnetic resonance imaging (MRI) can visualize tenosynovitis and a semiquantitative scoring system for tenosynovitis in the hand has previously been suggested1. In a multi-reader exercise, we aimed to assess the intra- and inter-reader agreement and responsiveness of a proposed OMERACT MRI tenosynovitis scoring system in the wrist and metacarpophalangeal (MCP) flexor tendons in the hands of RA patients.
Methods: Axial T1-weighted pre- and post-contrast fat-sat MRIs (0.8mm slice thickness) of the hand of 43 patients initiating rituximab therapy were obtained at baseline and after 3 (n=5), 6 (n=8), 9 (n=15) or 12 (n=15) months. The MRIs were read and scored twice on separate days with intermediate re-anonymization by 4 readers blinded to patient data but not to chronology. The tendons of 6 extensor and 3 flexor tendon compartments of the wrist and 4 flexor tendon compartments of the 2nd to 5th MCP joints were assessed. Tenosynovitis was defined as peritendinous effusion (PE) or post-contrast tenosynovial enhancement (PTE) on 3 consecutive slices. Pathologies were measured perpendicularly to the tendon at the thickest point of the effused or enhanced tenosynovium. Tenosynovitis was scored as follows: 0: no, 1: >0 but <1.5mm, 2: ≥1.5 but <3mm, 3: ≥3mm PE or PTE. Change in score over time was assessed using descriptive statistics and the Wilcoxon signed-rank test. Intra- and inter-reader agreement was calculated using intra-class correlation coefficients (ICC), percentage of exact and close agreement (PEA and PCA) and the smallest detectable change (SDC). Responsiveness to change was assessed using standardized response mean (SRM).
Results: The mean (SD) change in score between baseline and follow-up was -1.38 (2.84) for wrist, -0.94 (1.85) for MCP flexor tendons and -2.31 (4.63) for total score (all p<0.01). Intra- and inter-reader ICC for status scores were very good in all readers, except baseline scores in the MCP region in 1 reader. Intra-reader ICC for change scores were good to very good in all readers, and inter-reader ICC for status and change scores were very good in all readers. Intra-reader PEA for status and change scores was above 57% and PCA above 95% for all parameters. Inter-reader PEA was above 40% and PCA above 81% for all parameters. Intra-reader SDC was equal or below 3.0 and inter-reader SDC was below 2.0 in all readers. SRM was small to moderate (table 1).
Conclusion: The proposed OMERACT tenosynovitis scoring system showed high intra- and inter-reader agreement and small to moderate responsiveness for the wrist and MCP tendons and is a reliable tool for MRI-assessment of tenosynovitis in the RA hand. 1Haavardsholm et al. Ann Rheum Dis 2007;66(9):1216-20 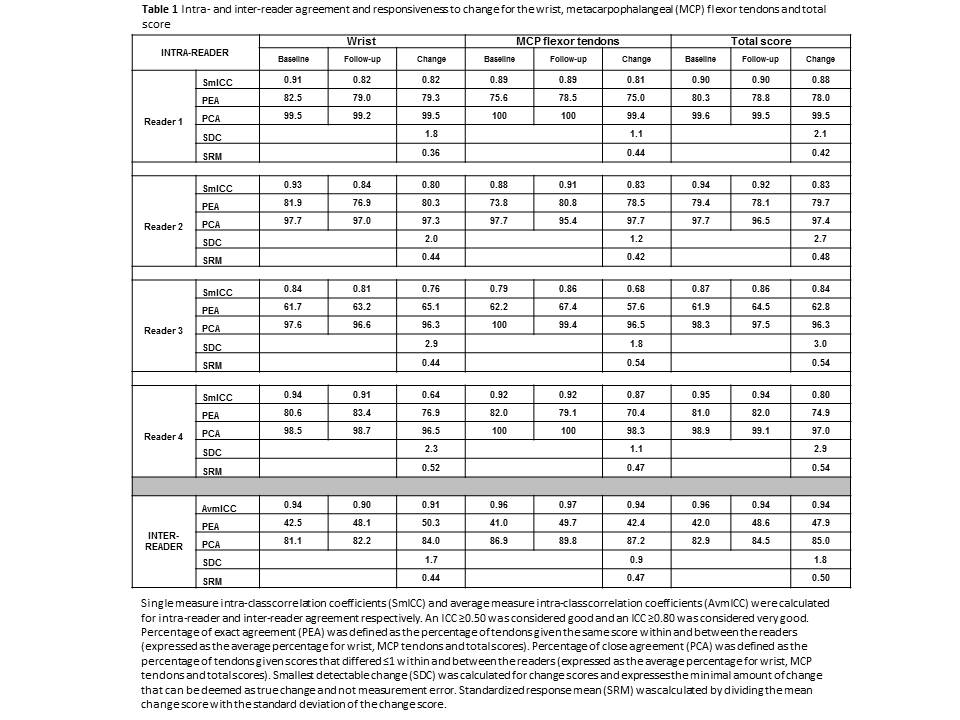
To cite this abstract in AMA style:
Glinatsi D, Bird P, Gandjbakhch F, Haavardsholm EA, Conaghan PG, Østergaard M. Reliability and Responsiveness of an Omeract Tenosynovitis Magnetic Resonance Imaging Scoring System for the Rheumatoid Arthritis Wrist and Hand [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/reliability-and-responsiveness-of-an-omeract-tenosynovitis-magnetic-resonance-imaging-scoring-system-for-the-rheumatoid-arthritis-wrist-and-hand/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/reliability-and-responsiveness-of-an-omeract-tenosynovitis-magnetic-resonance-imaging-scoring-system-for-the-rheumatoid-arthritis-wrist-and-hand/
