Session Information
Date: Sunday, November 8, 2015
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Axial Spondyloarthritis (axSpA) is often misdiagnosed or diagnosed late (average delay 8 to 11 years) since low back pain (LBP) is very common in general population and only 5% of those have axSpA. Effective screening and selective referral of high-risk patients (Pt) can help avoid this delay. There are no recommendations for a referral strategy for axSpA in the United States (US). We performed a systematic review to assess the effectiveness of various referral strategies on the final diagnosis of axSpA, and feasibility of their use in US health system.
Methods:
Pubmed and EMBASE search was performed to identify relevant articles using MeSH terms. After screening abstracts and titles of 135 retrieved articles, 9 full length articles were included for initial review. Three articles were excluded; 2 had different outcome and one was poor quality study. We included a single abstract since it describes the only available study in the US assessing a referral strategy. Final review included 6 full articles and 1 abstract. Data about referral source, referral strategy, Pt characteristics and outcomes were collected. Feasibility was determined by ease of the application of a strategy.
Results:
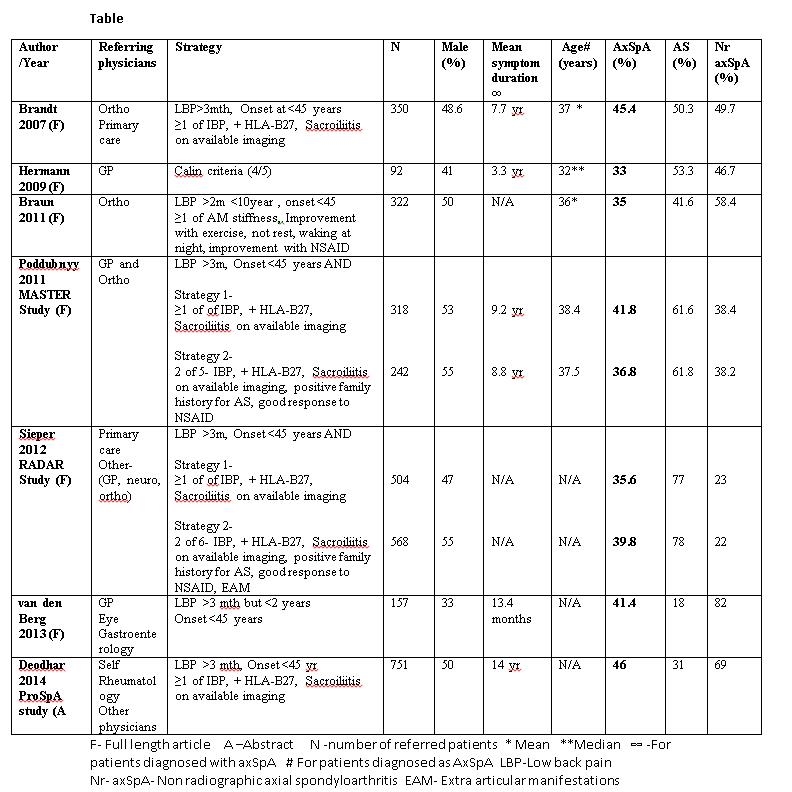
Most studies used “age at symptom onset <45 years and duration >3 months” as entry criterion (EC) for referral. Pt fulfilling EC only or EC plus combinations of spondyloarthritis (SpA) features (inflammatory back pain (IBP), HLA-B27 (B27), imaging sacroiliitis (iSI), good response to NSAIDS, family history of SpA, uveitis) were referred to rheumatologists. Commonest sources of referral were primary physicians, physical therapists and orthopedists. (See table) Application of simple (EC + 1 of 3 features) and complex strategies (EC + 2 of 5 or 2 of 6 features) produced similar results with 35-45% Pt finally diagnosed as axSpA. Even among studies that used only EC, 33 % to 41% of Pt were diagnosed to have axSpA. Simple strategy of fulfilling EC + 1 of 3 of IBP, B27 and iSI was found to be convenient, feasible and widely acceptable in multicenter studies. Presence of >1 SpA features was associated with higher likelihood of axSpA (24.6%, 44.9%, and 75.5 % for 1, 2 and 3 features respectively). As a single SpA feature in addition to EC, iSI, B27 and IBP were associated with final diagnosis of axSpA in 50%, 55% and 24% respectively, thus confirming low specificity of IBP.
Conclusion:
Referral strategies are effective tools for screening Pt with chronic back pain for presence of axSpA. Simple strategies work equally well compared to complex strategies. With appropriate application of any strategy, rheumatologist will need to see 2-3 Pt with chronic LBP to identify one Pt with axSpA. We believe that in the US, referring Pt with chronic LBP for >3 months, age of onset <45 years AND one of IBP, B27, iSI to rheumatologist for assessment of possible axSpA would be practical, with an acceptable efficacy.
To cite this abstract in AMA style:
Danve A, Deodhar AA. Referral Strategies for the Early Diagnosis of Axial Spondyloarthritis- a Systematic Review [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/referral-strategies-for-the-early-diagnosis-of-axial-spondyloarthritis-a-systematic-review/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/referral-strategies-for-the-early-diagnosis-of-axial-spondyloarthritis-a-systematic-review/