Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Infection is the leading cause of mortality and one of the most common causes of hospitalization in patients with systemic lupus erythematosus (SLE). Pneumocystis jirovecii pneumonia (PJP) is a highly morbid but preventable opportunistic infection in SLE patients. Prior studies have not investigated patient factors associated with PJP infection in SLE using an electronic health record (EHR) cohort. Using a real-world, EHR cohort, we assessed the frequency of PJP infection in SLE patients and patient factors associated with infection.
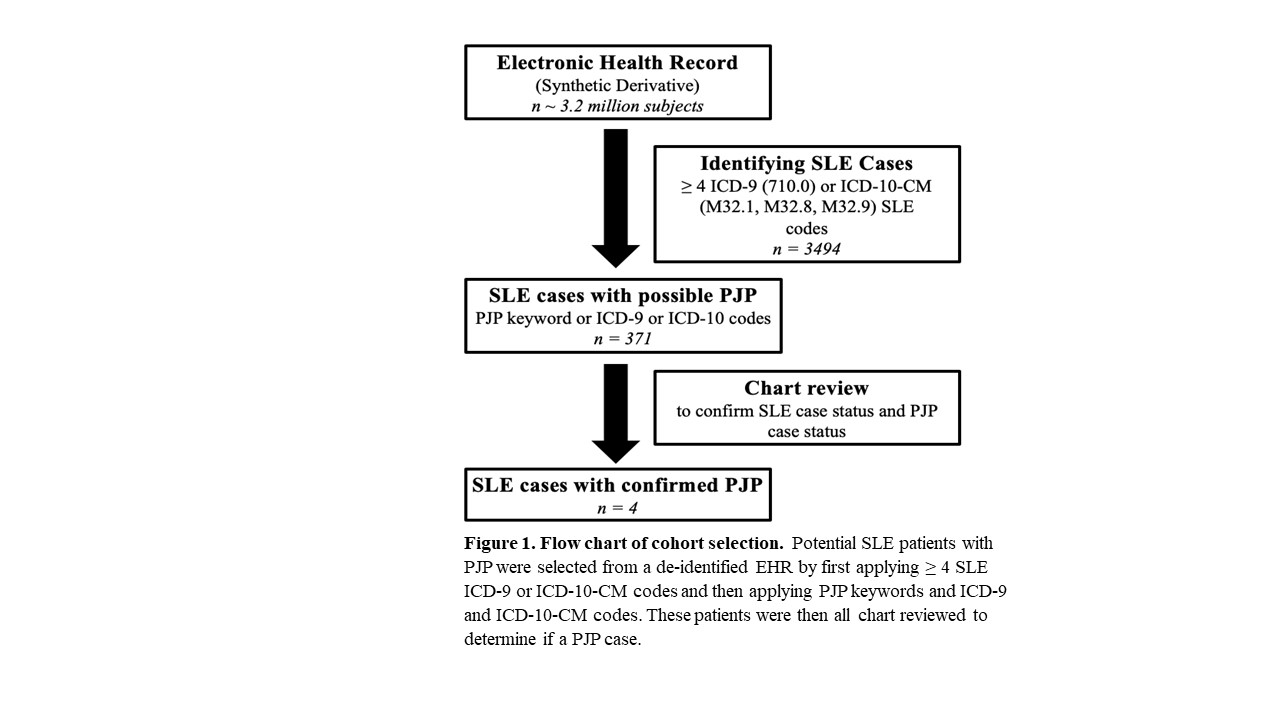
Methods: We identified potential SLE cases from a de-identified EHR called the Synthetic Derivative with over 3.2 million subjects with over 30 years of follow-up using a previously validated algorithm of 4 or more SLE ICD-9 or ICD-10 CM codes with a positive predictive value of 90%. Within this set, we then required either a PJP ICD-9 or ICD-10 CM code or PJP keywords. PJP keywords included “PJP”, “Pneumocystis jirovecii”, “Pneumocystis”, “PJP pneumonia”, or “pneumocystis pneumonia”. The cohort selection is summarized in Figure 1. Confirmed PJP infection was defined by positive immunofluorescence, polymerase chain reaction, or Gömöri methenamine silver staining on sputum or bronchoalveolar lavage specimen. We reviewed charts to collect data on demographics, SLE disease manifestations, medication exposure, laboratory values, and PJP prophylaxis use. We assessed for current and preceding 90-day cumulative dosing of corticosteroids at time of diagnosis from notes, inpatient and outpatient electronic prescribing systems, and phone messages. The current and recent use of non-steroid immunosuppressants over 90 days was recorded, as well as any co-morbid immunodeficiency.
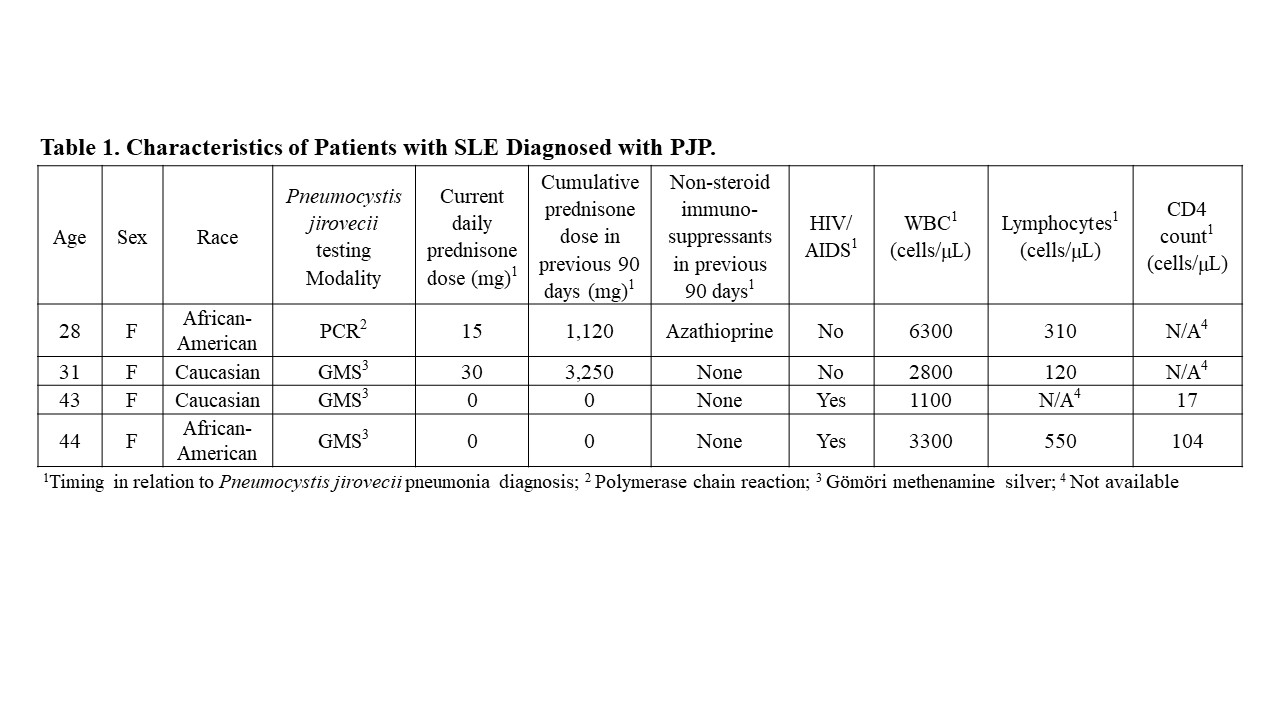
Results: We conducted chart review on 371 SLE patients with any mention of PJP from 1989 to 2020. A total of 119 patients underwent bronchoscopy for PJP testing, 16 underwent sputum sampling, and 10 underwent testing from other sites. We confirmed PJP infection in 4 of these patients. The characteristics of these patients, including relevant therapies and laboratory evaluation, are summarized in Table 1. Two of the 4 patients were infected with human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) with CD4 lymphocyte counts less than 200 cells/mL. Neither of these patients had been exposed to any steroids or non-steroid immunosuppressive therapy in the 90 days preceding PJP diagnosis. Of the 2 SLE patients without HIV/AIDS, both had significant lymphopenia in addition to significant recent steroid exposure. None of the 4 patients were on PJP prophylaxis.
Conclusion: Using a large EHR cohort, 2 SLE patients without co-morbid HIV/AIDS were identified as having PJP. Both patients were on moderate doses of corticosteroids, with one on a non-steroid immunosuppressant, and neither on PJP antimicrobial prophylaxis. With 2 confirmed cases of PJP in non-HIV/AIDS SLE patients in over 30 years at a large academic institution, PJP seems to be a rare complication in SLE. This rarity may contribute to lack of well-defined risk factors for PJP infection or formal recommendations for PJP prophylaxis in SLE patients.
To cite this abstract in AMA style:
Boone B, Barnado A. Rarity of Pneumocystis Jirovecii Pneumonia in Patients with Systemic Lupus Erythematosus Using a Real-world, Electronic Health Record [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/rarity-of-pneumocystis-jirovecii-pneumonia-in-patients-with-systemic-lupus-erythematosus-using-a-real-world-electronic-health-record/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rarity-of-pneumocystis-jirovecii-pneumonia-in-patients-with-systemic-lupus-erythematosus-using-a-real-world-electronic-health-record/