Session Information
Date: Sunday, October 26, 2025
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Radiographic sacroiliitis is an important indicator of axial involvement psoriatic arthritis (PsA), but only little is known about factors associated with progression of sacroiliitis. This study aimed to assess radiographic sacroiliitis progression in PsA and identify demographic, clinical, and genetic factors influencing its progression.
Methods: We included individuals from an observational Psoriatic Arthritis cohort (1978–2025). Pelvic radiographs were collected biannually. The Sacroiliitis Sum Score (SSS, 0–8) was calculated as the total sacroiliitis grades for the left and right sacroiliac joints, based on the modified New York (mNY) radiographic system. Radiographs were assessed by consensus. Progression was defined as an increase in the SSS by at least 1 point. Linear mixed models were used to evaluate factors influencing sacroiliitis progression, with the change in SSS as the outcome variable.
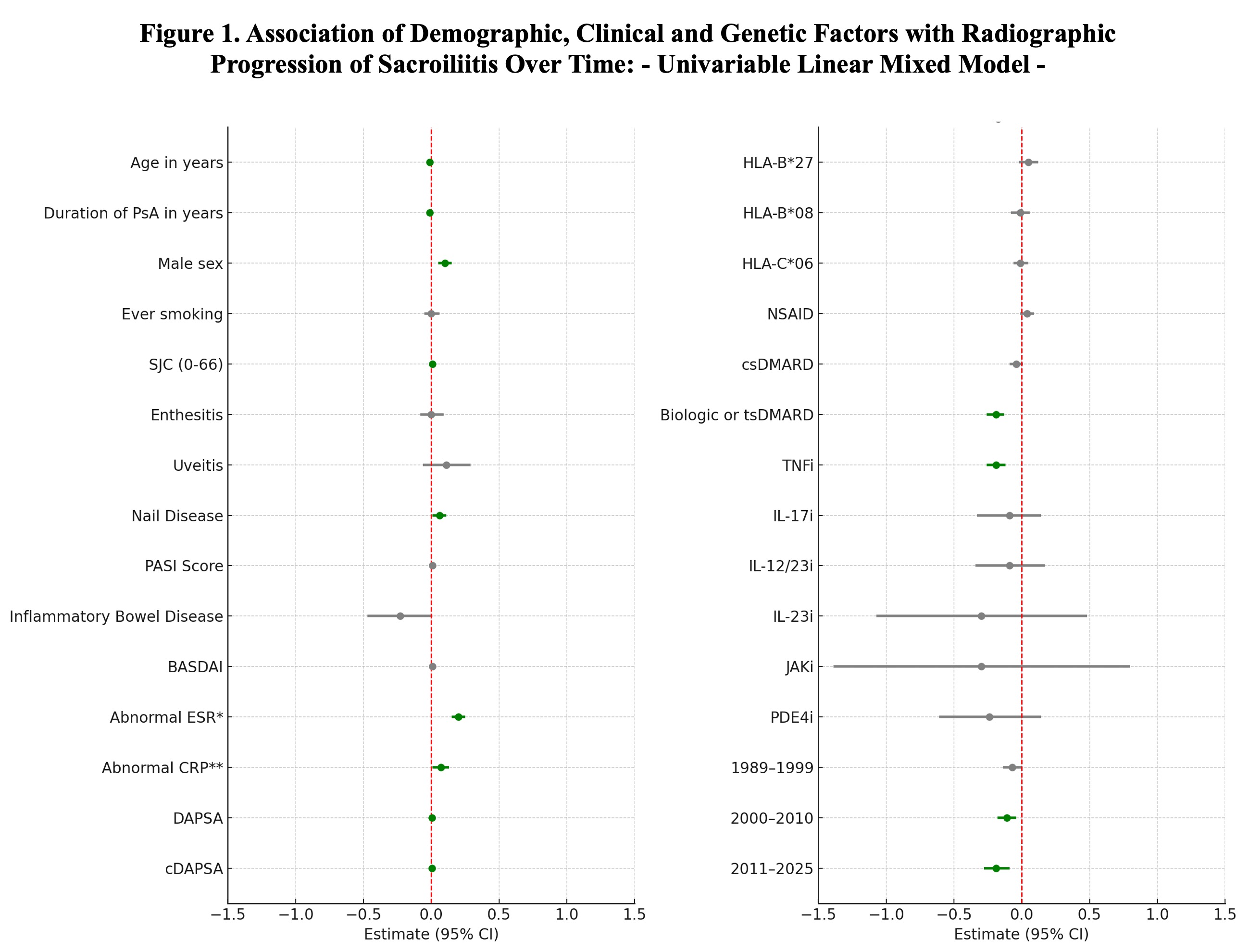
Results: A total of 1,554 patients without an SSS of 8, with a median follow-up duration of 6 years (range: 0.00–13.30), were included. Among them, 475 (30.6%) showed progression of radiographic sacroiliitis (SSS change ≥1). At baseline, 22% of all patients had sacroiliitis according to the mNY criteria, and 20% were HLA-B*27 positive.Variables positively associated with progression included male sex, swollen joint count (SJC), Psoriasis Area and Severity Index (PASI), nail psoriasis, abnormal ESR, abnormal CRP, Disease Activity Index for PsA (DAPSA), and clinical DAPSA (Figure 1). Longer PsA duration was negatively associated with progression. HLA alleles, including HLA-B*27, were not significantly associated with progression.Patients who received biologic or targeted synthetic DMARDs had significantly lower odds of progression. TNF inhibitors demonstrated a protective effect against sacroiliitis progression compared to other treatments. An analysis of the calendar effect showed a decline in sacroiliitis progression over time, with a greater reduction observed in the 2011–2025 period.In multivariable analysis, male sex remained significantly associated with greater sacroiliitis progression, while biologic and targeted synthetic therapies continued to show a protective effect. (Figure 2)
Conclusion: Radiographic sacroiliitis progression occurred in one-third of patients. In univariable and multivariable analyses, male sex was associated with greater progression, while biologic and targeted synthetic therapies were protective.
To cite this abstract in AMA style:
Carrizo Abarza V, Mehta P, Kharouf F, Gao S, Gladman D, Chandran V, Poddubnyy D. Radiographic Sacroiliitis Progression in Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/radiographic-sacroiliitis-progression-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/radiographic-sacroiliitis-progression-in-psoriatic-arthritis/

.jpg)