Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The purpose of this study was to examine differences in perceptions of psoriatic arthritis (PsA) disease burden as well as various aspects of care across racial/ethnic groups.
Methods: Survey questions assessing PsA patient insights regarding their disease burden and quality of care were developed. From September to October 2022, surveys were deployed to 455 PsA patients either through a leading advocacy organization email list (n = 420) or an additional national patient survey organization (n = 35). Self-reported race/ethnicity was recorded. If patients selected both “white” and another racial/ethnic group, they were included in both groups in the analysis.P values were calculated using the chi-square or Fisher’s Exact tests for counts less than 5.
Results: The age of patients ranged from 28 to 91 years. Three hundred ninety-one identified as white and 76 identified with a racial/ethnic minority group (29 African American/Black, 20 Asian/Pacific Islander, 14 Hispanic/Latinx, 8 Native American/Alaska Native, 5 “Other”).
Racial/ethnic minority PsA patients were less likely to be diagnosed within 12 months from the onset of symptoms (50% vs 71%; P < 0.001) and more frequently uninsured (8% vs. 1%; P < 0.001) compared to white patients. Racial/ethnic minority patients more often had self-described severe disease vs. white patients (41% vs. 14%; P < 0.001) and extreme impact on quality of life and emotional well-being (25% vs. 6%; P < 0.001).
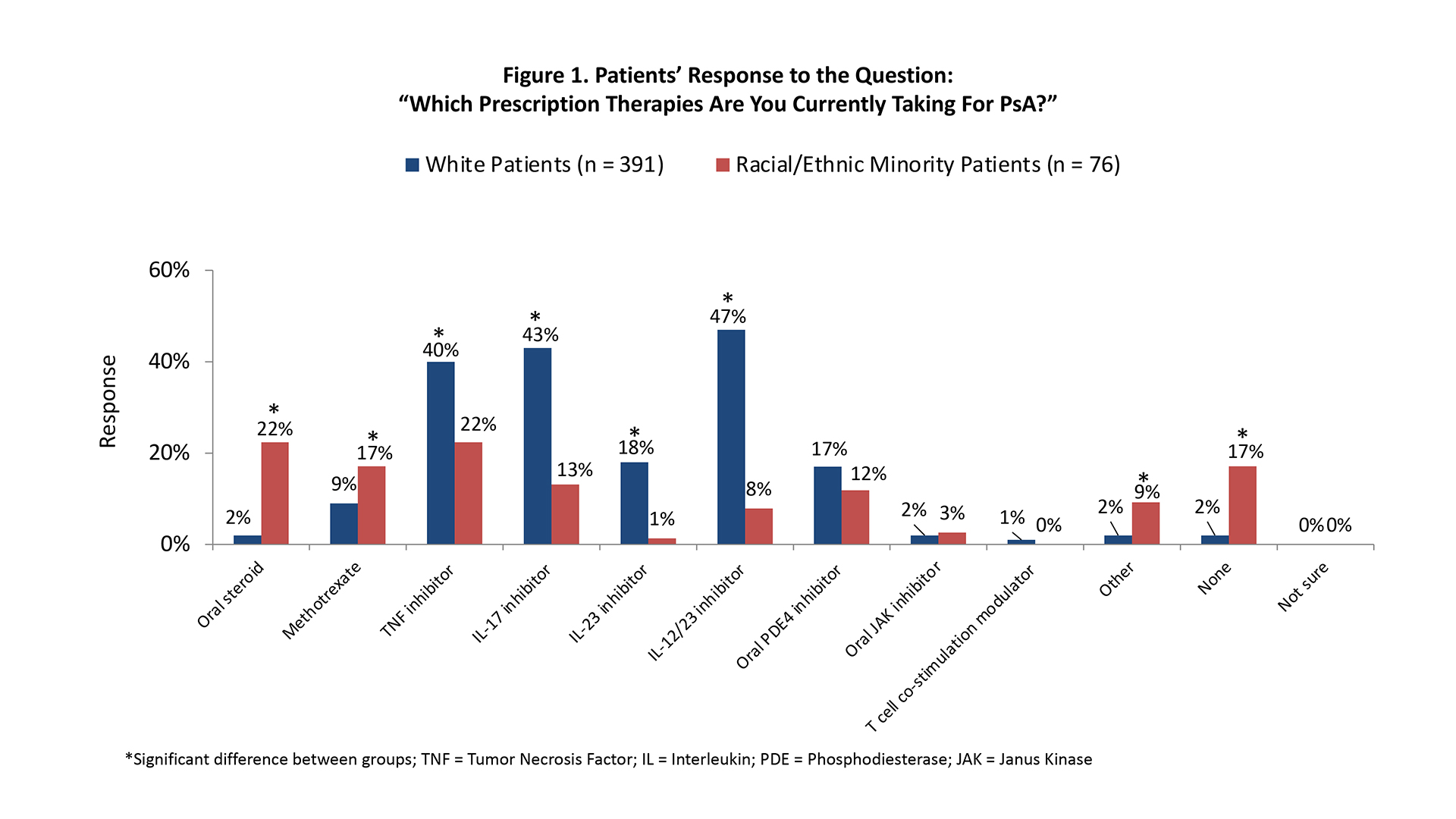
Regarding treatment, racial/ethnic minority PsA patients were less often prescribed a biologic and more frequently received oral glucocorticoids, methotrexate, or no prescription medications compared to white PsA patients (Figure 1). Also less frequent among racial/ethnic minority patients were high levels of knowledge/familiarity with targeted agents such as injectable biologics or oral small molecule inhibitors (42% vs. 81%; P < 0.001) and high satisfaction with treatment (39% vs. 77%; P < 0.001). Financial barriers to managing PsA were four-fold more common in racial/ethnic minority patients (26% vs. 7%; P < 0.001); the difference in concern for risks of medications was similarly significant (29% vs. 3%; P < 0.001).
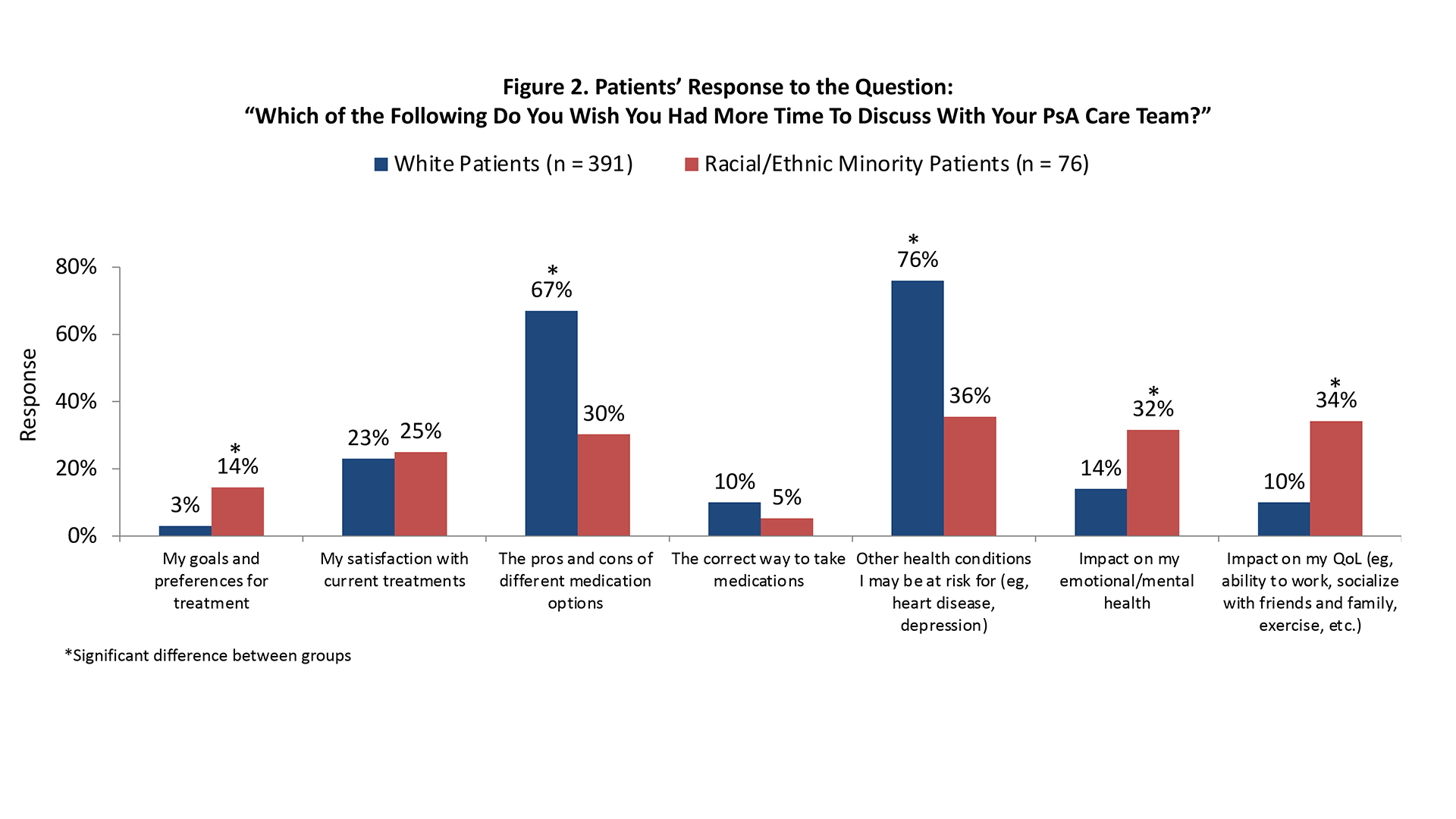
Gaps in communication with the PsA care team were also observed. Racial/ethnic minority patients were less likely to feel that they were very/extremely involved in shared decisions regarding their care (60% vs. 82%; P < 0.001). When asked what they wished they had more time to discuss with their care team, racial/ethnic minority PsA patients requested various aspects of the impact of the disease as well as goals and preferences for treatment (Figure 2). Notably, the advantages and disadvantages of different treatment options and comorbidities were a lower priority in racial/ethnic minority patients despite a higher percentage of comorbid disease (Figure 2).
Conclusion: These survey findings confirm racial/ethnic disparities across the spectrum of PsA disease from time to diagnosis to treatment, and underscore the dissatisfaction with overall care. There is a need for more time to be spent on educating individuals with PsA to enable shared decisions and improved understanding of therapeutic options.
To cite this abstract in AMA style:
Navarro-Millán I, Kerr G, Carter J, Simone L, Nelson M. Racial/Ethnic Differences in Psoriatic Arthritis Patient Responses Regarding Disease Burden, Treatment, and Communication with Care Team [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/racial-ethnic-differences-in-psoriatic-arthritis-patient-responses-regarding-disease-burden-treatment-and-communication-with-care-team/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-ethnic-differences-in-psoriatic-arthritis-patient-responses-regarding-disease-burden-treatment-and-communication-with-care-team/