Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Significant racial disparities exist in SLE outcomes. Few studies have examined modifiable factors intrinsic to physician/patient encounters that may contribute to such disparities. We aimed to explore potential areas for intervention to reduce racial disparities with a focus on patient self-efficacy and the quality of patient-provider interactions.
Methods: Cross-sectional data were collected from consecutive patients meeting ACR or SLICC criteria for SLE and actively being treated at a tertiary lupus clinic. Patient-provider interaction was measured using the Interpersonal Processes of Care survey (IPC-29), which has 7 domains on a 5-point Likert scale. General self-efficacy, self-efficacy for managing medications and treatments, and patient-reported health status were measured using Patient-Reported Outcomes Measurement Information System (PROMIS) short forms. Additional demographic and clinical information were gathered by survey and chart review. Bivariate analyses compared characteristics of Caucasian vs. minority patients. Linear regression analysis was performed to assess race-stratified association of SLICC damage scores with age, education, IPC-29 and patient self-efficacy scores.
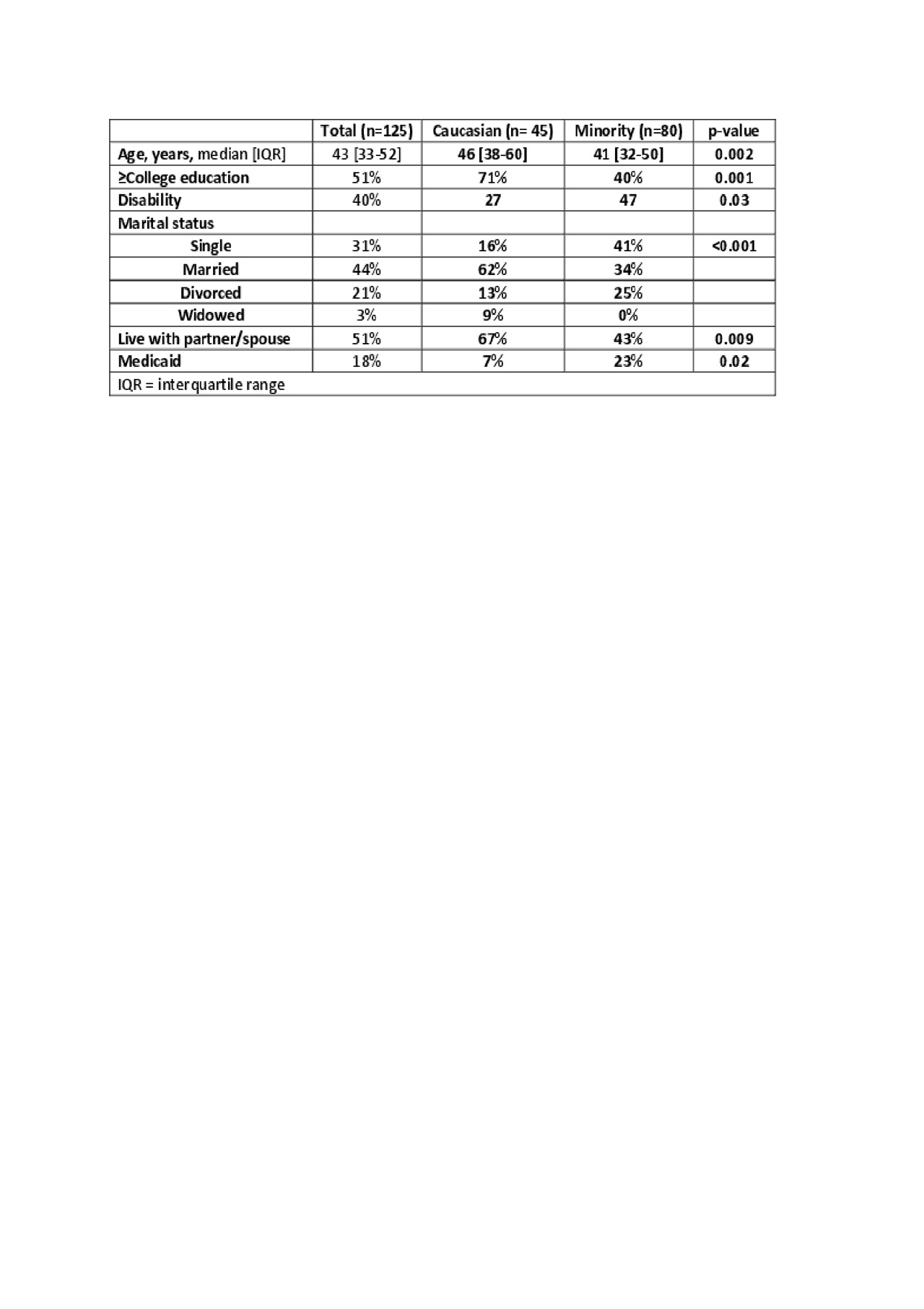
Results: 125 patients were enrolled (36% Caucasian, 61% African American, 3% other). Minorities compared to Caucasians were younger, less likely to be college educated, married, live with partner or spouse, and more likely to be on Medicaid (table 1). Minorities reported less fatigue and better social health, took more complex rheumatic medication regimens, had higher SLEDAI, lower fibromyalgia symptom severity, and a trend for higher damage scores (table 2). Minorities rated more hurried communication with their providers, and there were no racial differences in self-efficacy scores. Among minorities, more hurried communication, lower general self-efficacy, and lower self-efficacy in managing medications and treatments were each associated with higher SLICC damage scores, but among Caucasians only older age (β=0.09 95% CI 0.06-0.14, p< 0.001) and ≤ college education (β= -2.6, 95% CI -3.8- -1.4, p< 0.001) were associated with higher damage scores (figure 1).
Conclusion: Minorities were from more disadvantaged sociodemographic backgrounds and had more active SLE. Overall, scores for patient-rated interactions with physicians in this selective sample were very good. However, minorities reported more hurried communication with their providers.
To cite this abstract in AMA style:
Sun K, Eudy A, Rogers J, Criscione-Schreiber L, Doss J, Sadun R, Clowse M. Racial Disparities in Factors Associated with SLICC Damage Score Among Patients with SLE [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/racial-disparities-in-factors-associated-with-slicc-damage-score-among-patients-with-sle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-in-factors-associated-with-slicc-damage-score-among-patients-with-sle/