Session Information
Date: Monday, November 13, 2023
Title: (1013–1032) Healthcare Disparities in Rheumatology Poster II: Socioeconomic Determinants
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
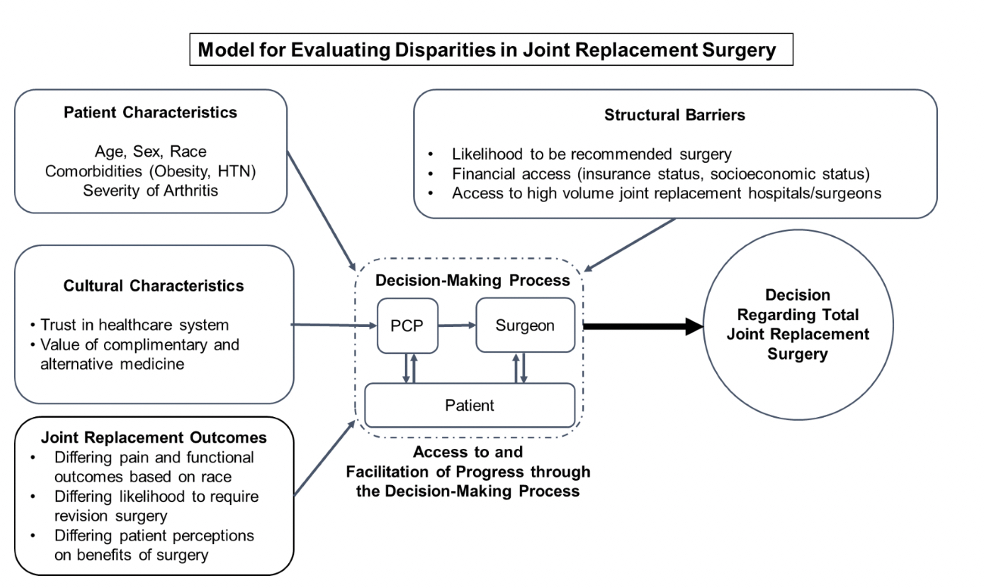
Background/Purpose: Despite the documented efficacy of joint replacement surgery (JRS) for the management of refractory hip or knee osteoarthritis (OA), multiple studies have documented lower rates of JRS among Black patients with refractory hip or knee OA. The purpose of this research is to investigate how differences in patient characteristics, cultural characteristics, outcomes after joint replacement surgery (JRS), and structural barriers between Black and White patients may affect the decision to undergo JRS and how those decisions contribute to differences in utilization in JRS.
Methods: Original searches ran on April 8, 2019, April 7, 2020 and updated October 11, 2022 in the following databases: Ovid MEDLINE (ALL – 1946 to Present); Ovid EMBASE (1974 to present); and The Cochrane Library (Wiley). Our population of interest was black patients with hip and/or knee OA, our comparator was white patients with hip and/or knee OA, and our primary outcome was disparities in decisions regarding JRS. We registered the protocol under the PROSPERO international register and followed the Preferred Reporting Items of Systematic reviews and Meta-Analyses (PRISMA) guidelines. We included any articles which fit within our model (Figure 1).
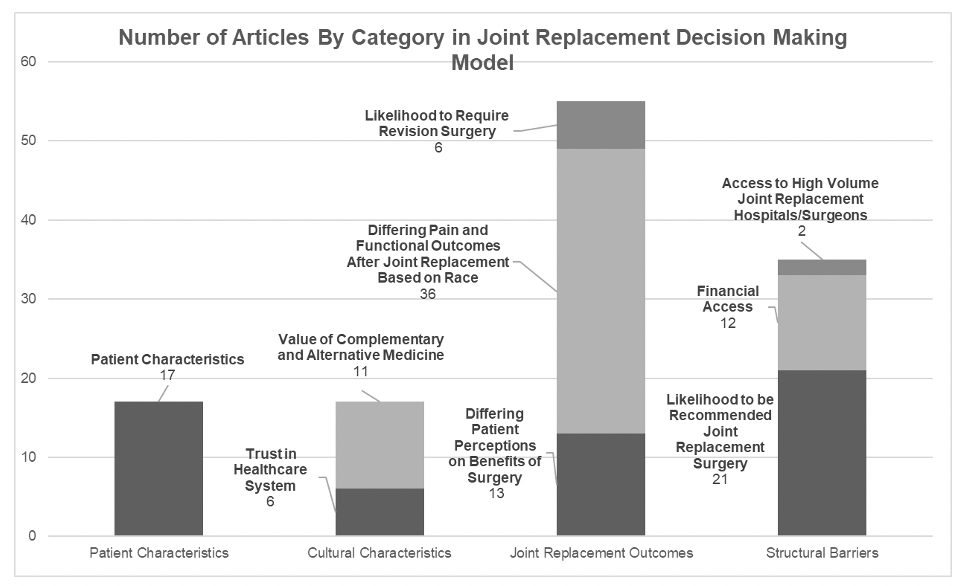
Results: Searches across the chosen databases retrieved 21,390 results, 14,252 after results after de-duplication, 351 pulled for full text, and 96 selected for inclusion in this review. We then categorized these articles using our conceptual model (Figure 1): 17 in patient characteristics, 17 in cultural characteristics, 55 in joint replacement outcomes and 35 in structural barriers. We further subclassified articles within each category, as outlined in Figure 2.
Relative to white patients, Black patients had higher levels of pain catastrophizing, disability, lower levels of physical function, longer length of stay post total knee arthroplasty (TKA) and total hip arthroplasty (THA), increased ED visits post THA and TKA, decreased proportions of JRS performed as outpatients, higher rates of discharge to post-acute care facilities, and higher risk of revision after TKA. In certain analyses, the effect of race was shown to be mediated by socioeconomic disadvantage and comorbidity burden.
Conclusion: Preliminary review of the data finds that Black patients undergo JRS at lower rates than White patients. While some of this difference can be explained by lower preference for JRS vs. other arthritis treatments among Black patients, there are significant structural, financial, provider and patient factors that contribute to this difference. Some of these factors could be targeted for intervention to improve access to JRS for Black patients. The articles included for review primarily investigated differences in joint replacement outcomes and structural barriers, with less research studying baseline patient and cultural characteristics.
To cite this abstract in AMA style:
Krall M, Good S, Brantner C, Pearce-Fisher D, Goodman S, Parks M, Sculco P, Kahlenberg C, Premkumar A, Demetres M, FitzGerald J. Racial Disparities Between Black and White Patients in Joint Replacement Surgery: A Systematic Review [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-between-black-and-white-patients-in-joint-replacement-surgery-a-systematic-review/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-between-black-and-white-patients-in-joint-replacement-surgery-a-systematic-review/