Session Information
Session Type: Abstract Session
Session Time: 3:45PM-4:00PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a leading cause of end-stage kidney disease (ESKD) in young women, particularly among racial and ethnic minorities. Kidney transplantation is the preferred treatment for SLE-related ESKD, yet disparities in transplant access and outcomes persist. In 2014, the Kidney Allocation System (KAS) was revised to improve equity in organ distribution. This study evaluates racial and ethnic disparities in kidney transplant outcomes among SLE patients during the 10 years before and after the 2014 KAS revision.
Methods: We conducted a retrospective cohort study using the United Network for Organ Sharing (UNOS) Standard Transplant Analysis and Research (STAR) files. Adult patients with SLE who received kidney transplants between 2005-2024 were identified and stratified into two cohorts: Pre-revision (2005–2014) and Post-revision (2015–2024).We compared demographics, mean waitlist days, 1-year graft failure, and 1-year mortality across cohorts, stratified by race/ethnicity (Black, White, Hispanic, Other).Multivariable logistic regression estimated the adjusted odds of 1-year graft failure and mortality by race/ethnicity (White as reference), adjusting for age, sex, HLA mismatch level, insurance type, and other clinical covariates.
Results: A total of 10,547 SLE kidney transplant recipients were included (4,255 pre-revision; 6,292 post-revision) (Table 1). Before KAS revision, Black patients had the longest mean waitlist time (938.8 vs 629.9 days for White patients). Post-revision, they had the largest decrease in wait time (–143.2 days; p< 0.001), while other groups showed no significant change (Table 2). All groups experienced increased 1-year graft failure post-revision, with the greatest increases among Black (+14.7%) and Hispanic (+13.0%) recipients. No significant changes were observed in 1-year mortality across groups.In adjusted post-revision models, Black (OR 1.46, 95% CI 1.22–1.75; p< 0.001) and Hispanic (OR 1.28, 95% CI 1.04–1.56; p=0.017) recipients had significantly higher odds of graft failure compared to White recipients (Table 2). "Other" had lower odds (OR 0.72, 95% CI 0.54–0.97; p=0.029). Only Hispanic patients had significantly lower odds of 1-year mortality (OR 0.29, 95% CI 0.12–0.69; p=0.005).
Conclusion: Although the 2014 KAS revision reduced wait times for Black recipients, it was associated with increased 1-year graft failure across all groups, particularly among Black and Hispanic patients There were no significant corresponding changes in mortality. The reasons for these trends are likely multifactorial and may include changes in immunologic matching, or shifts in perioperative care and follow-up practices. The findings suggest that while the KAS revision may have improved access to transplantation, it may have inadvertently introduced new risks for certain populations. Further investigation is needed to understand the mechanisms driving these outcome disparities and to inform future refinements to transplant policy.
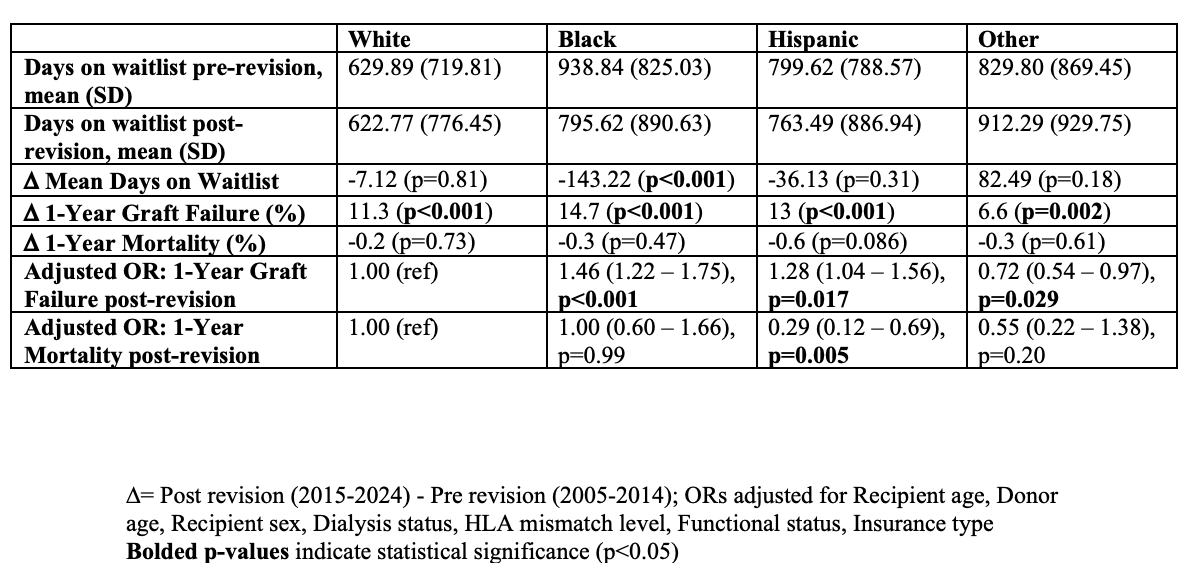 Table 1: Demographic and Clinical Characteristics of SLE Patients Who Received Kidney Transplants Before and After the 2014 Kidney Allocation System (KAS) Revision
Table 1: Demographic and Clinical Characteristics of SLE Patients Who Received Kidney Transplants Before and After the 2014 Kidney Allocation System (KAS) Revision
.jpg) Table 2: Changes in Kidney Transplant Wait Times and Outcomes in SLE Patients Following the 2014 Kidney Allocation System (KAS) Revision, by Race/Ethnicity
Table 2: Changes in Kidney Transplant Wait Times and Outcomes in SLE Patients Following the 2014 Kidney Allocation System (KAS) Revision, by Race/Ethnicity
To cite this abstract in AMA style:
Salia S, Mensah B, Mamoh U, Hedayati G, Baffoe-Bonnie T, Morny J, Haas C. Racial and Ethnic Disparities in Kidney Transplant Outcomes Among Patients With Systemic Lupus Erythematosus (SLE): A 20-Year Analysis Spanning Before and After the 2014 Kidney Allocation System Revision [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/racial-and-ethnic-disparities-in-kidney-transplant-outcomes-among-patients-with-systemic-lupus-erythematosus-sle-a-20-year-analysis-spanning-before-and-after-the-2014-kidney-allocation-system-revis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-and-ethnic-disparities-in-kidney-transplant-outcomes-among-patients-with-systemic-lupus-erythematosus-sle-a-20-year-analysis-spanning-before-and-after-the-2014-kidney-allocation-system-revis/
