Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Over 450,000 primary total hip arthroplasties (THA) are performed each year. One major indication for primary THA is the presence of osteoarthritis (OA). Patient characteristics, insurance payer status, and regional and hospital level factors can lead to disparities in outcomes and costs of primary THA in patients with OA. We aimed to examine the association of these factors to extended lengths of stay and increased hospital costs after primary THA.
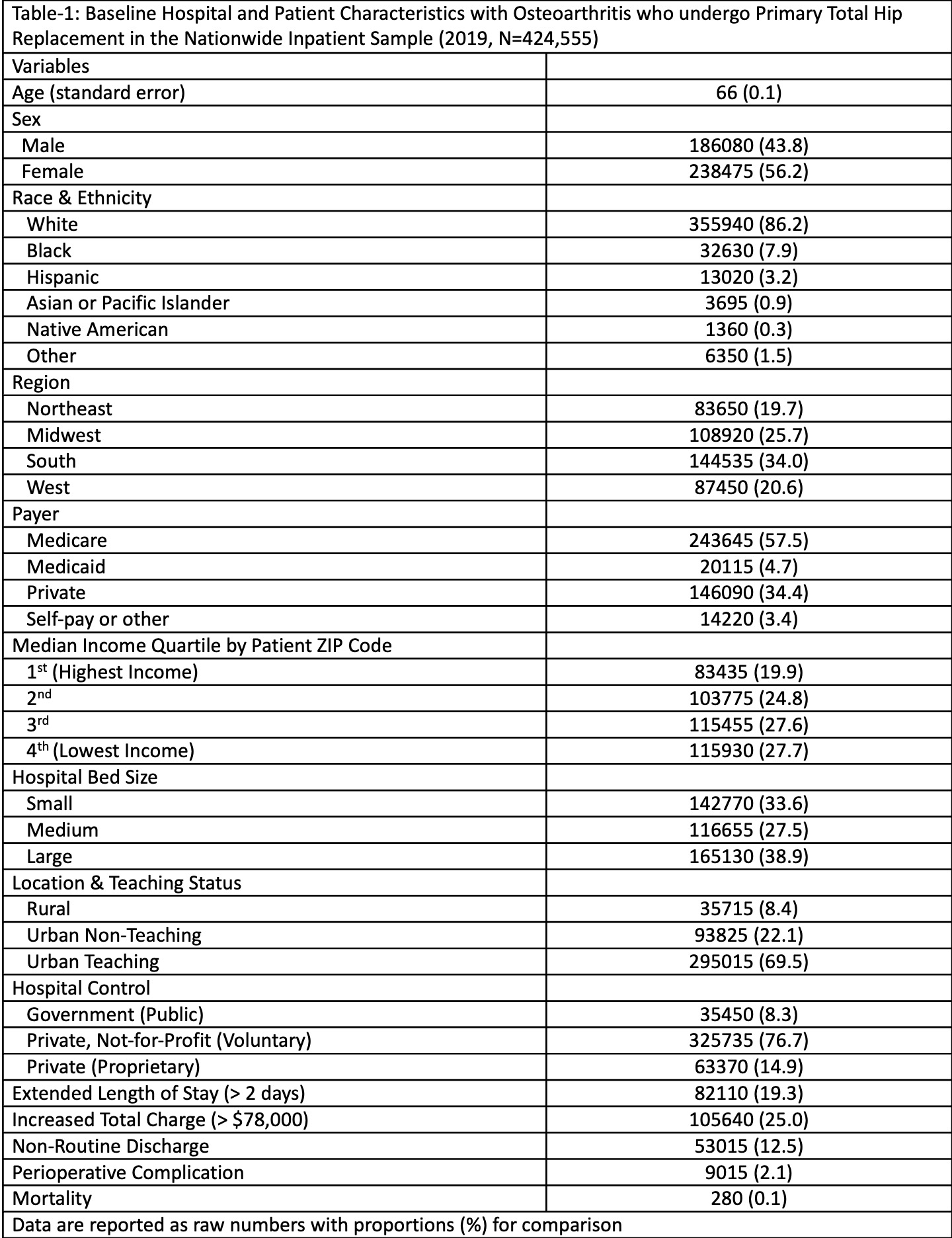
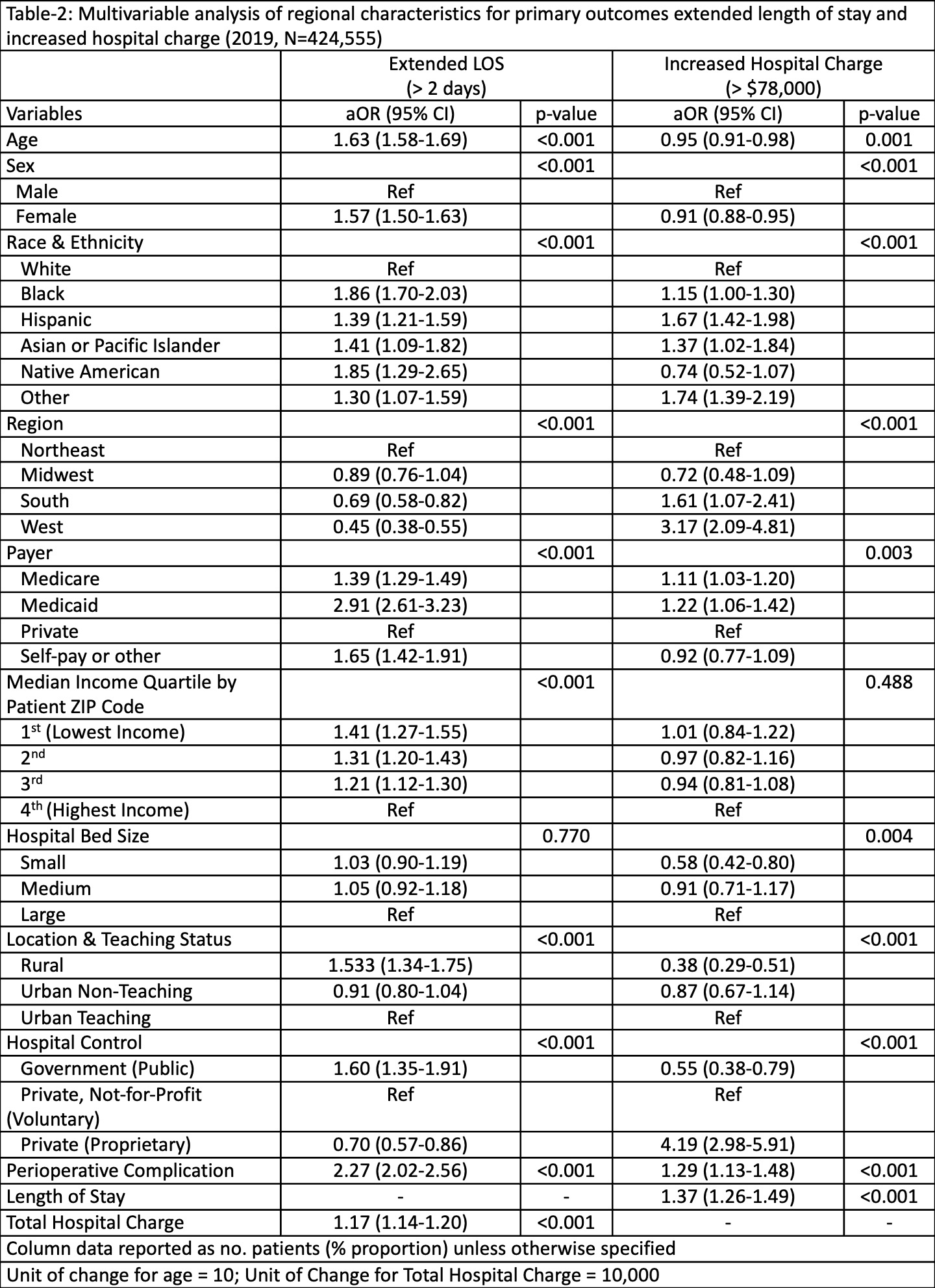
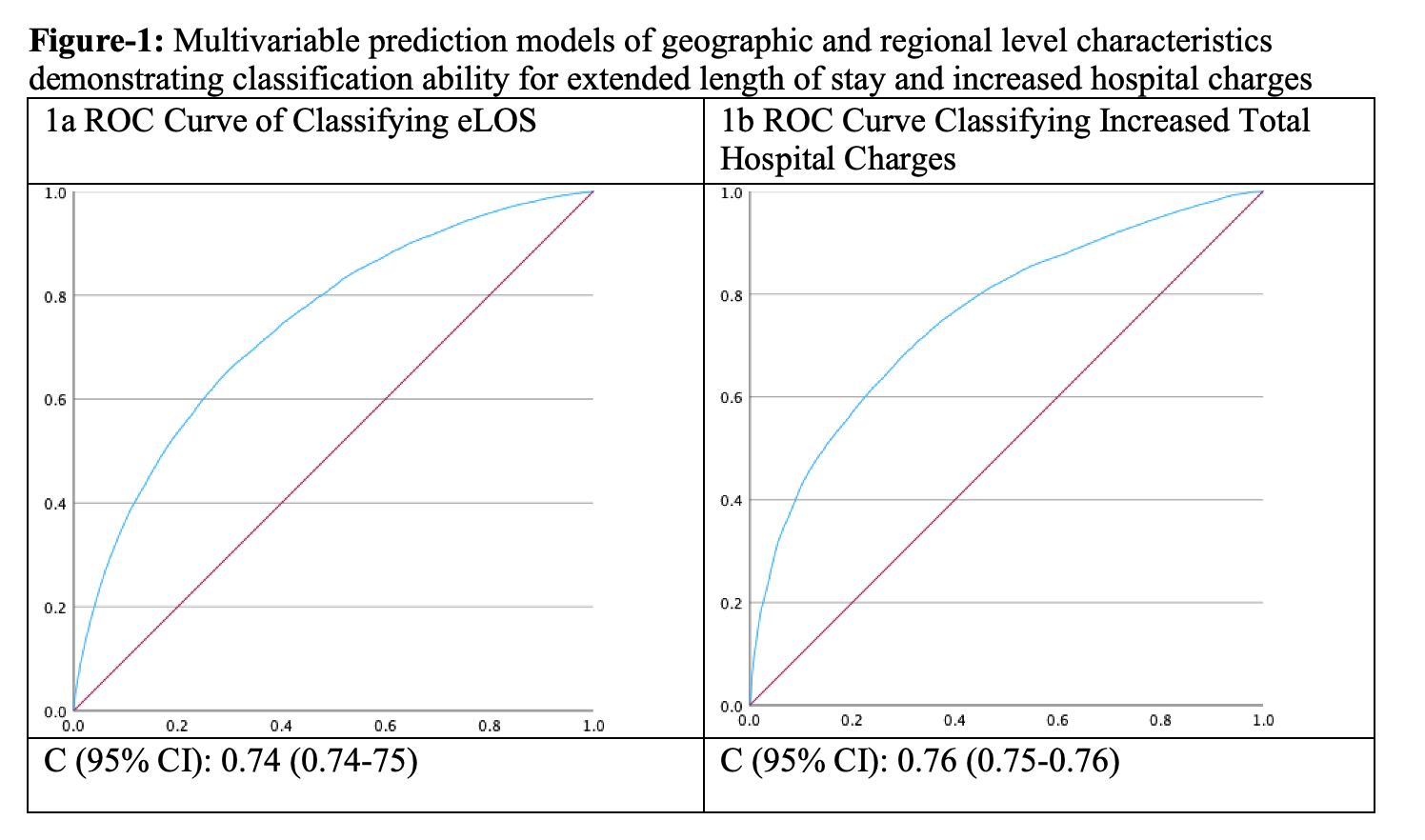
Methods: We utilized the National Inpatient Sample (NIS) to identify patients with OA who underwent primary THA in 2019. Diagnoses and procedures were identified using the International Classification of Disease (ICD-10) codes. We stratified healthcare/resource utilization by the occurrence of an extended length of stay (eLOS) and the presence of an increased hospital charge (IHC), i.e., the upper quartile each outcome. Univariate and multivariable analyses compared patient-level, regional, and hospital characteristics associated with an eLOS or IHC. Predictive probabilities from multivariable analyses were used in Area Under the Curve (AUC) analysis.
Results: There were 424,555 patients with OA who underwent primary THA in 2019. Patient race/ethnicity, Medicaid or Medicare payer status, income, age/sex and nearly all regional, and hospital, characteristics were independently associated with eLOS (ROC C-statistic = 0.74). Significant independent predictors for IHC were race & ethnicity (p < 0.001), hospital region (p < 0.001), hospital location & teaching status (p < 0.001), and hospital control (p < 0.001). The ROC curve classifying IHC had a C-statistic of 0.76.
Conclusion: Patient race/ethnicity and insurance payer status are important determinants of longer LOS for primary THA hospitalizations in the US. Well-known geographical and hospital-level disparities are negatively associated with the outcomes and costs of primary THA in patients with OA. Policy and other interventions targeting these factors may help reduce utilization for elective THA.
To cite this abstract in AMA style:
Rumalla K, Chandrupatla S, Singh J. Race, Payer, and Hospital Factors Are Associated with Post-primary Total Hip Arthroplasty Healthcare Utilization [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/race-payer-and-hospital-factors-are-associated-with-post-primary-total-hip-arthroplasty-healthcare-utilization/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/race-payer-and-hospital-factors-are-associated-with-post-primary-total-hip-arthroplasty-healthcare-utilization/