Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Quantitative clinical measures and indices such as DAS28, CDAI, SLEDAI, BASDAI, are designed to assess inflammation, reflecting a goal to prevent long-term damage, and are effective in patients selected for high activity in clinical trials. However, in rheumatology routine care, many patients have clinically important damage of joints and other organs and/or distress, as fibromyalgia, manifested by similar signs and symptoms to those seen in inflammation, i.e., functional disability, pain, fatigue, high patient global assessment and tender joint counts, but damage and distress are not recorded quantitatively. Patients with many non-rheumatic diseases, e.g., diabetes, also may have clinically important damage and/or distress, which is usually ignored unless presenting an acute problem, as signs and symptoms differ from the “gold-standard” biomarker (hemoglobin A1c) that is predominant in clinical decisions1. By contrast, rheumatology signs and symptoms of damage and/or distress may be similar to those of inflammation. The expertise of the rheumatologists may be viewed to recognize whether findings are primarily a result of inflammation, damage, and/or distress, and possibly 2 or 3 of these variables. This process involves greater complexity in the examination room than application of a gold-standard biomarker acquired (and reimbursed) elsewhere, and may provide a rationale for higher reimbursement, but is not recorded quantitatively. We examined a hypothesis that many routine care patients have findings of 2 or 3 components of inflammation, damage and/or distress to explain a physician global assessment (DOCGL).
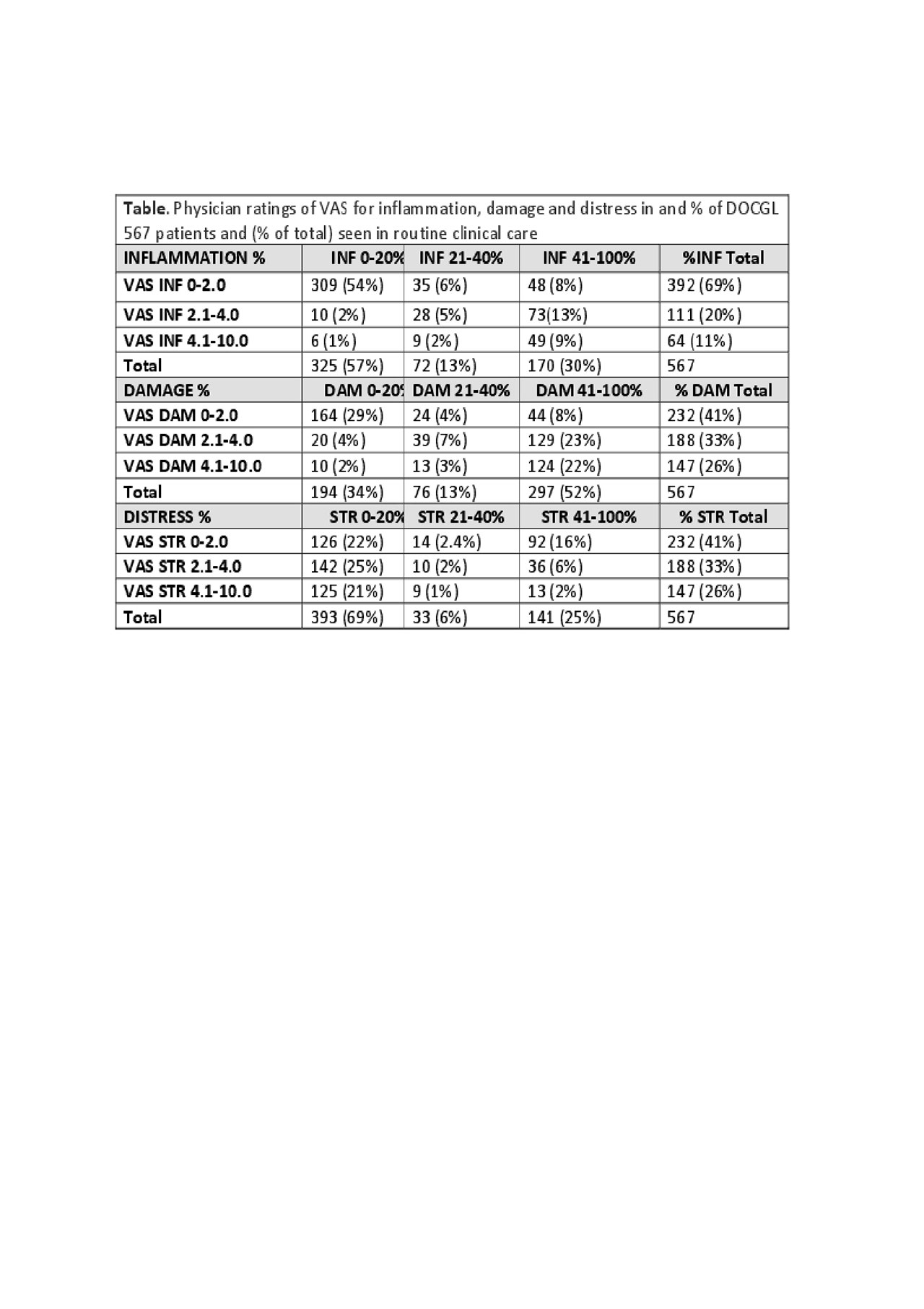
Methods: Rheumatologists at one academic site complete a RheuMetric checklist which includes a physician global assessment (DOCGL) scores on a 0-10 visual analogue scale (VAS), and 3 additional 0-10 VAS subscales for inflammation (DOCINF), damage (DOCDAM), and distress (DOCSTR), as well as the % of DOCGL attributed to each of the 3 variables (Total=100%) to explain the basis for DOCGL. VAS scores classified as 0-2, 2.1-4, 4.1-10, and % of DOCGL classified as 0-20, 21-40, 41-100% were compared using descriptive statistics and cross-tabulations.
Results: In 567 unselected patients, DOCINF was >4/10 in 11%, vs 26% each for DOCDAM and DOCSTR (Table), indicating that 37% (=100-11-26-26) had at least 2 clinically important (VAS >2) variables, and 9% all 3 (data not shown). The proportion of patients in whom DOCGL was regarded as explained >40% by inflammation was 30%, vs damage in 52% and distress in 25% (Table). Therefore, a single basis for signs and symptoms was most prominent only in a minority of patients.
Conclusion: Quantitative rheumatologist VAS indicate that organ damage and patient distress often are as prominent as inflammation, and patients may have 2 or 3 bases for signs and symptoms. If confirmed at other sites, the results suggest a rationale to record a VAS for inflammation, damage, and distress, to document greater complexity of rheumatology encounters vs those based on a “gold standard” biomarkers, and possible adjustments in reimbursement for quantitative data to document the expertise of rheumatologists.
- Castrejon et al. Arthritis Care Res. 2012;64(8):1250-5.
To cite this abstract in AMA style:
Pincus T, Castrejon I, Block J. Quantitative Physician Global Assessment of Damage And/or Distress, in Addition to Inflammation, at Routine Rheumatology Care: Documenting the Complexity of Rheumatology Patient Encounters as a Rationale for Possible Higher Reimbursement? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/quantitative-physician-global-assessment-of-damage-and-or-distress-in-addition-to-inflammation-at-routine-rheumatology-care-documenting-the-complexity-of-rheumatology-patient-encounters-as-a-ration/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/quantitative-physician-global-assessment-of-damage-and-or-distress-in-addition-to-inflammation-at-routine-rheumatology-care-documenting-the-complexity-of-rheumatology-patient-encounters-as-a-ration/