Session Information
Date: Monday, October 27, 2025
Title: (1248–1271) Patient Outcomes, Preferences, & Attitudes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with rheumatic diseases (RD) often experience chronic pain, along with comorbid depression and anxiety, which can be addressed using behavioral health (BH) interventions for motivating behavior change and increasing self-management skills. Despite potential benefits, efforts to integrate BH services into rheumatology clinics have been limited. We developed and piloted a single-arm BH program integrated within a rheumatology clinic to evaluate feasibility and trends towards improved patient-reported outcomes (PRO).
Methods: During their clinic visit, adult patients with RD were invited to participate in a pilot BH program. Interested patients were asked to select up to 3 BH goals of interest from a goal elicitation tool (Figure 1). Those who selected at least 1 of the 3 target goals that the BH specialist would focus on were eligible to participate in the telephone-based intervention, which consisted of up to 8, brief, patient-centered sessions, utilizing techniques such as motivational interviewing and mindfulness meditation combined with psychoeducation and supplemental apps/videos. PROs for pain interference (PEG-3), pain catastrophizing, depression/anxiety (PHQ-4) and PROMIS measures of fatigue, quality of life (QoL), physical function, sleep and social satisfaction were collected at baseline and during the final BH session. Depending on the normality of distribution, Wilcoxon signed-rank or student T-tests were used to compare baseline and post-intervention scores.
Results: We enrolled 54 participants, 45 completed the baseline assessment, and 39 engaged in at least 1 BH session beyond baseline. Of these, 28 completed the program (i.e., completed a final assessment session). Among the completers, 79% were women and white. Osteoarthritis (32%), rheumatoid arthritis (21%) and psoriatic arthritis (18%) were the most frequent rheumatologic diagnoses. Fifty percent of the sample had a mental health diagnosis code. Most participants (52%) focused on the goal “Improve My Mood/ Manage Stress & Anxiety” and completed the program in 8 sessions (IQR 6, 8). At baseline (n=28), average PEG-3 score was 3.69/10 and PHQ-4 score was 3.32/12. There was improvement in pre-post mean change scores for PEG-3, pain catastrophizing, PHQ-4, fatigue, sleep and QoL; however, no improvement was noted in social satisfaction or physical function (Table 1).
Conclusion: In this pilot study, recruitment and delivery of an integrated BH program was feasible in a busy rheumatology clinic. We found promising trends toward improvement in PROs for several domains, including pain, pain catastrophizing and depression/anxiety. These results warrant future evaluation with a fully powered randomized controlled trial.
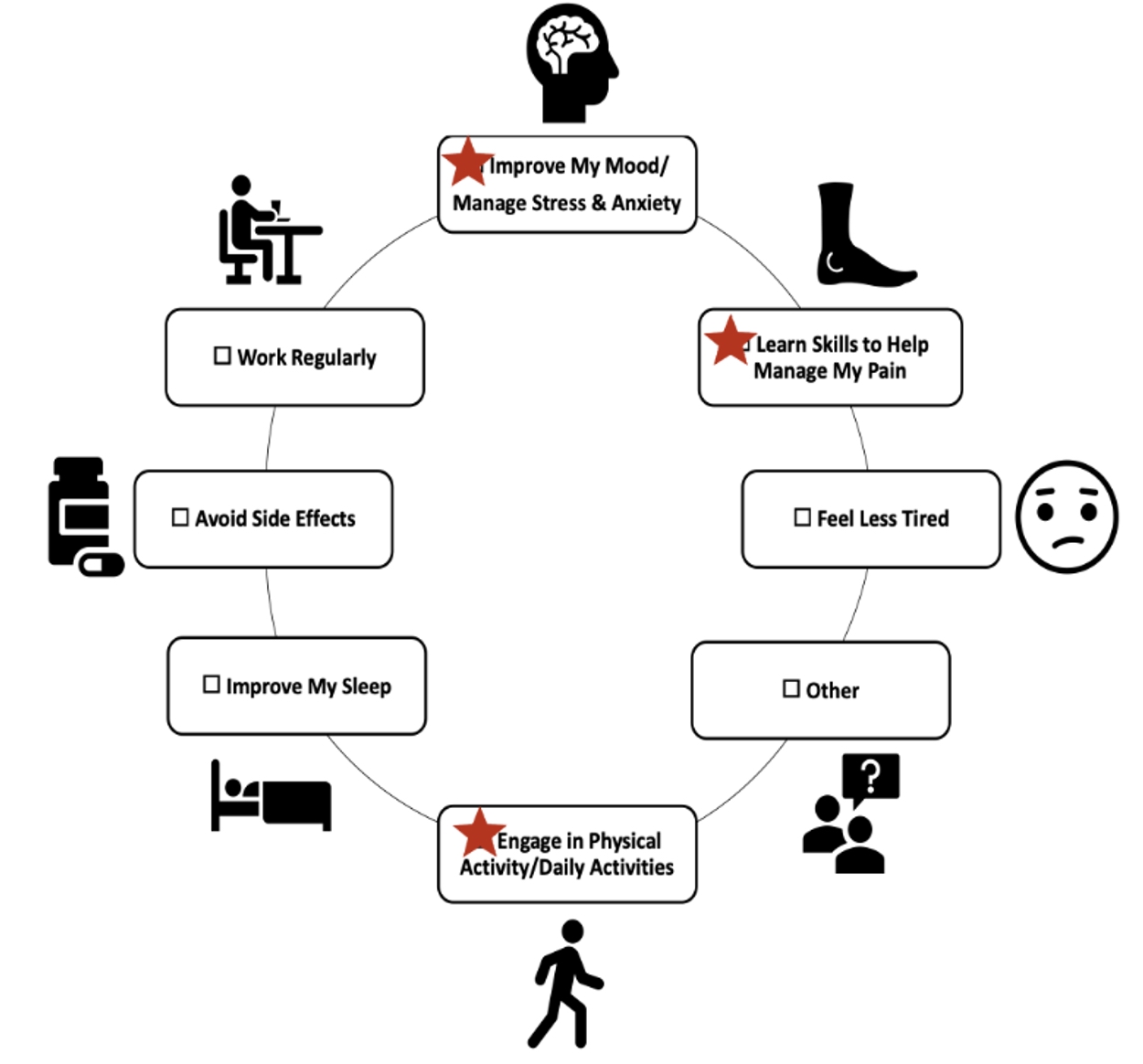 Figure 1. Goals Wheel. Stars indicate BH services offered.
Figure 1. Goals Wheel. Stars indicate BH services offered.
.jpg) Figure 2. Patient Reported Outcomes (PRO) pre-post mean change scores, Nf28; *indicates statistical significance
Figure 2. Patient Reported Outcomes (PRO) pre-post mean change scores, Nf28; *indicates statistical significance
To cite this abstract in AMA style:
Teaw S, Link-Malcolm J, Ghebranious Farag M, Patterson D, Foster J, Bereket S, Wahid U, Bajaj P, Solow E, Barton J, Makris U. Quantitative Analysis of a Pilot Study: Integrating Behavioral Health Services for Patients with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/quantitative-analysis-of-a-pilot-study-integrating-behavioral-health-services-for-patients-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/quantitative-analysis-of-a-pilot-study-integrating-behavioral-health-services-for-patients-with-rheumatic-diseases/
