Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Antisynthetase syndrome is characterized by fever, myositis, interstitial lung disease (ILD), inflammatory arthritis, mechanic’s hands, and Raynaud phenomenon. The most commonly reported form of antisynthetase syndrome has been associated with anti-Jo1 antibody and ILD is a major determinant of prognosis. However, the presence of pulmonary hypertension (PH) in anti-Jo1 syndrome had not been systematically evaluated in the past.
Methods: We conducted a retrospective chart review of patients with anti-Jo1 syndrome. Patients were evaluated both for ILD and/or PH. ILD was diagnosed on the basis of high resolution CT (HRCT) scan of lungs and PH had to be confirmed on right heart catheterization (RHC). The pattern and severity of ILD on HRCT scan was graded by a radiologist and each lung lobe was individually quantified with a score from 1 to 4 according to percentage of lobar involvement. A score of 1 represented <25% lobar involvement, 2: ≥ 25% but < 50%, 3: ≥ 50 % but < 75%, and 4: ≥ 75% involvement. Summation of individual lobar scores provided the overall ILD severity score. Fibrosis (reticular and honeycomb scores) and inflammation indices (ground glass opacity and mixed score) were also calculated (Ooi et al. Acta Radiologica. 2003).
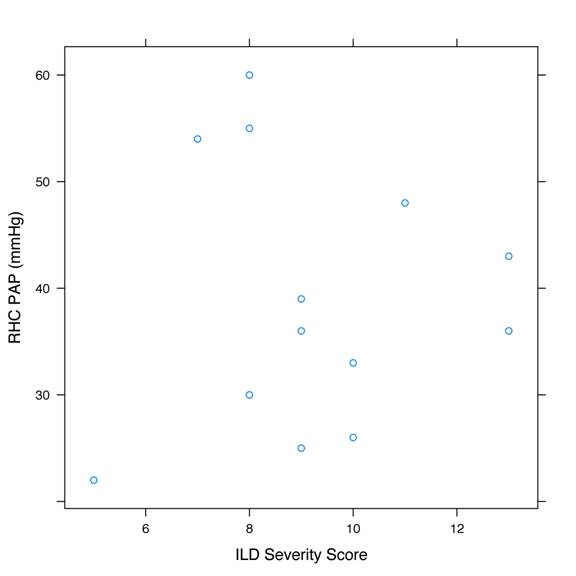
Results: We identified 116 patients with positive anti-Jo1 antibody, of which 13 were found to have RHC-confirmed PH and were included in this study. All 13 patients also had ILD. Mean age at diagnosis of antisynthetase syndrome was 51 years and mean age at diagnosis of pulmonary hypertension was 58 years. Of the 13 patients, 8 had mild PH (mean pulmonary artery pressure (mPAP): 25-40 mmHg), 4 had moderate PH (mPAP: 41-55 mmHg), and 1 had severe PH (mPAP: >55 mmHg). The predominant type of lung injury observed in these patients was inflammation, not fibrosis. For the same degree of ILD severity (Figure 1), there was significant variability in the severity of PH, indicating that PH in anti-Jo1 syndrome is not solely secondary to ILD, but is also a result of an independent inflammatory and/or fibro-proliferative process affecting the pulmonary microvasculature. The correlations between mPAP and overall ILD severity, inflammation index, or fibrosis index were not statistically significant.
Conclusion: Our findings suggest that chronic hypoxic pulmonary vasoconstriction or vascular obstruction/destruction associated with progressive ILD are not the sole mechanisms in the pathogenesis of PH in anti-Jo1 syndrome. It is likely that an obliterative pulmonary vasculopathy (possibly resulting from proliferation of endothelial and vascular smooth muscle cells) co-exists and plays an important role in the pathogenesis. Therefore, it may be appropriate to consider routine screening of anti-Jo1 syndrome patients at the onset of disease and periodically thereafter, in order to have maximum impact of vasoactive therapy on the outcome.
Figure 1
Disclosure:
N. Syed,
None;
R. Yadav,
None;
C. O’Rourke,
None;
S. Chatterjee,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-hypertension-in-anti-jo1-syndrome/