Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) is a chronic progressive inflammatory arthropathy associated with psoriasis (PsO). PsA places a considerable burden, adversely affecting health-related quality of life (HRQoL).
So far, all studies evaluating effectiveness and outcomes of PsA management have focused on arthritis while the impact on the skin component has served as a secondary endpoint. Hence, there is a knowledge gap on how both components interact with each other and impact patient-perceived dermatology-specific HRQoL.
This study evaluates the patient-perceived burden of skin disease in a PsA cohort.
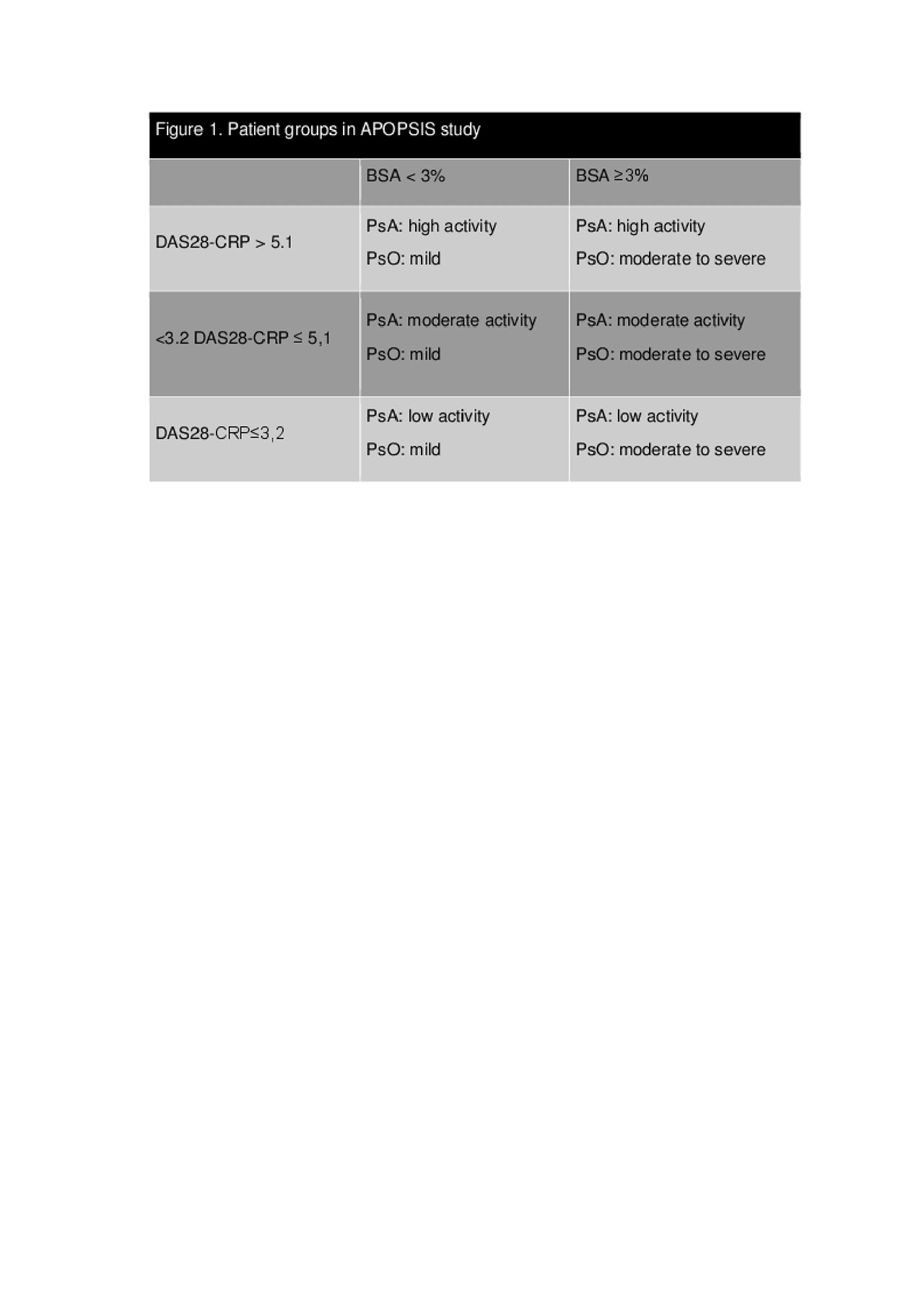
Methods: This was a multicenter, single-country, cross-sectional observational study primarily aiming to evaluate the importance of skin disease to Greek PsA patients adjusting for arthritis activity, in a routine clinical practice setting. Patients were classified into three groups according to their arthritis activity, which was defined using the DAS28 cut-off points: DAS28-CRP≤ 3.2 (low); DAS28-CRP >3.2 to ≤5.1 (moderate); and DAS28-CRP >5.1 (high). Within each arthritis group, patients were further sub-divided based on PsO severity, defined by the Body Surface Area (BSA) affected by PsO using a cutoff of 3% (Figure 1). PsO-dependent HRQoL was measured with the Dermatology Life Quality Index (DLQI). The primary endpoint was the mean difference in DLQI score between patients with BSA< 3% (mild PsO) versus patients with BSA ≥ 3% (moderate-to-severe PsO) within each of the defined PsA activity groups. A two-way factorial Analysis of Variance (ANOVA) was used to evaluate the difference of DLQI measurements between PsO severity levels in each PsA activity group.
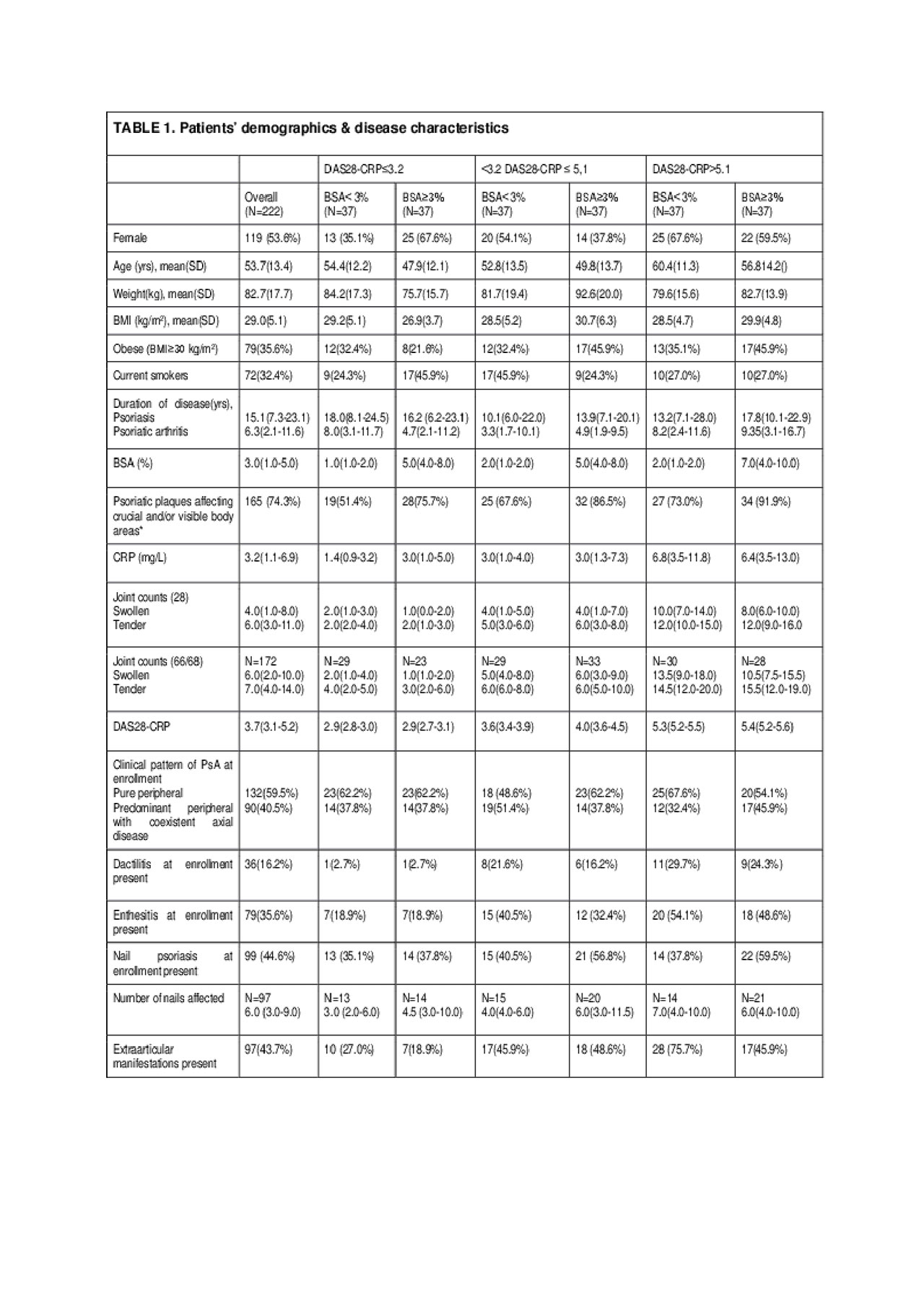
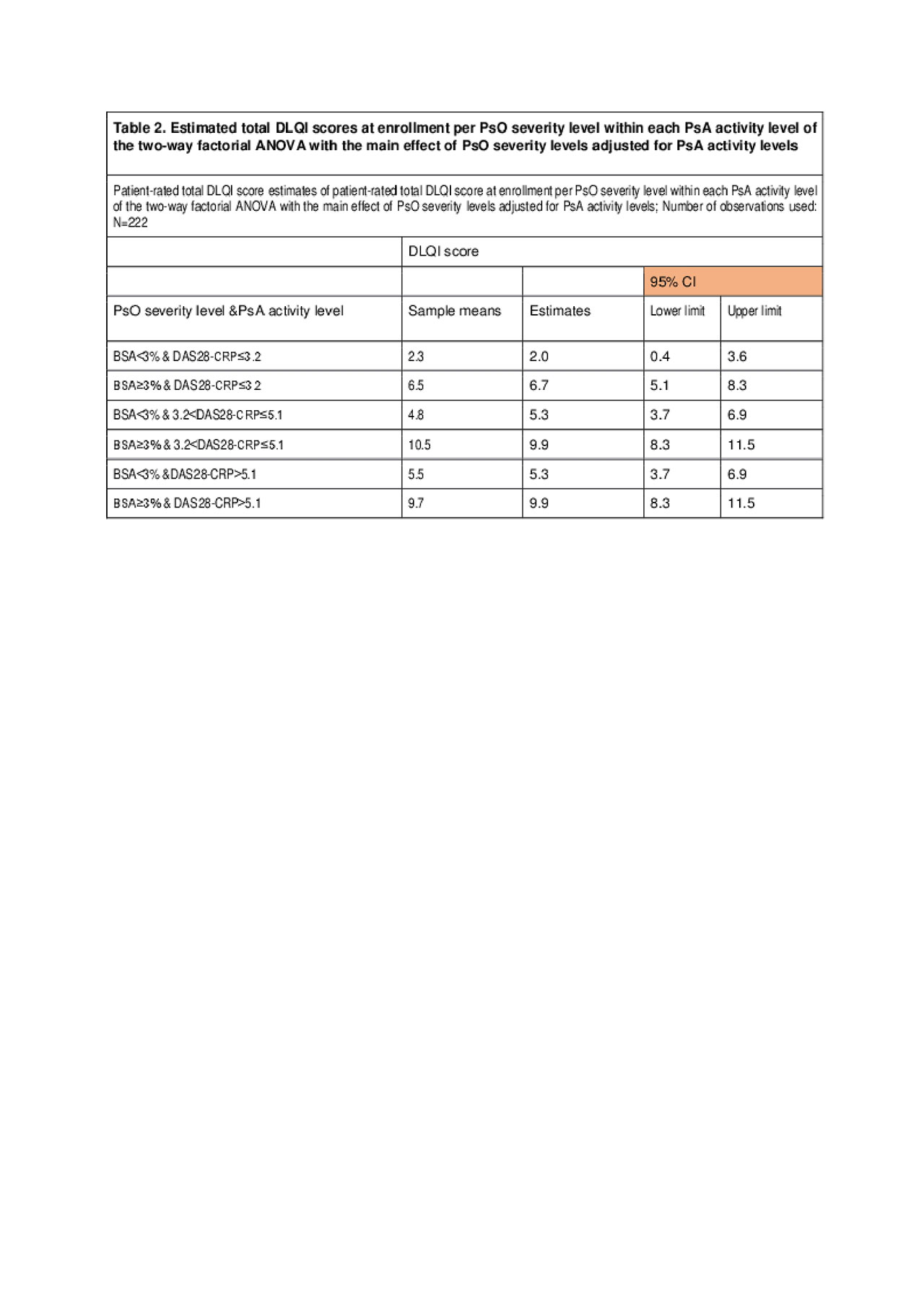
Results: Overall, 222 patients with purely peripheral or predominantly peripheral joint involvement were enrolled. All patients were Caucasian with a mean (SD) age of 53.7 (13.4) years. The median BSA was 3.0% (IQR: 1.0-5.0), and the median DAS28-CRP score was 3.7 (IQR: 3.1-5.2). Psoriatic plaques affected high impact sites, i.e. hands, feet, face, neck, scalp, genitals/groin, and intertriginous areas in 74.3% (165/222) of patients (Table1). With regard to the primary endpoint, results showed that the interaction between PsO severity and PsA activity overall was not statistically significant (p=0.672). However, a statistically significant main effect of PsO severity on DLQI was identified (p< 0.001) showing that the mean DLQI difference between PsO levels is the same in each of the PsA activity groups. The two-way factorial ANOVA mean difference in DLQI total scores between patients with ‘moderate-to-severe’ and patients with ‘mild’ PsO was estimated to be 4.7 (95% CI: 3.1-6.3; p< 0.001) across all three PsA activity levels (Table2). Moreover, patients with PsO plaques at high impact sites reported DLQI scores 2.4 points (95% CI: 0.4-4.3; p=0.019) higher than those for patients without plaques at such sites.
Conclusion: This study provides novel real-world evidence demonstrating that PsO severity negatively impacts the dermatology-specific HRQoL independent of the PsA disease activity. In addition, PsO localization at high impact sites (excluding nails) adversely affects dermatology-specific HRQoL.
To cite this abstract in AMA style:
Athanassiou P, Theodoridou A, Koukli E, Georgountzos A, Vlachoyiannopoulos P, Kallitsakis I, Sakkas L, Matsouka Dapola A, Gazi S, Georgiou P, Gorecki P, Gkamaloutsos C. Psoriasis Impact on Patient-Reported Outcomes in Psoriatic Arthritis in a Real-World Setting: Results from the APOPSIS Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/psoriasis-impact-on-patient-reported-outcomes-in-psoriatic-arthritis-in-a-real-world-setting-results-from-the-apopsis-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/psoriasis-impact-on-patient-reported-outcomes-in-psoriatic-arthritis-in-a-real-world-setting-results-from-the-apopsis-study/