Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Long-term use of proton pump inhibitors (PPI) have been linked to safety concerns. In a previous retrospective analysis, a potential association between PPI use and calcinosis in systemic sclerosis (SSc) was identified. We explored this in a prospective study.
Methods: Data from prospectively recruited patients were collected by patient survey, clinical review and medical records. Calcinosis was graded; size (+= <1cm, ++= ≥1 ≤3cm, +++= >3cm) and number of sites involved (NSI) (I = 1 body site, II = 2-3, III = >3). A total daily PPI equivalent dose (TDED) was calculated for each patient. We computed PPI exposure score (PPE) by multiplying the total duration of use in years (y) by TDED. For analysis, PPE was categorised into four groups; 0 = no exposure, 1 = up to 5y, 2 = 6-10y, 3 = >10y. Fishers exact test assessed categorical variables. Logistic regression assessed association between calcinosis and independent variables.
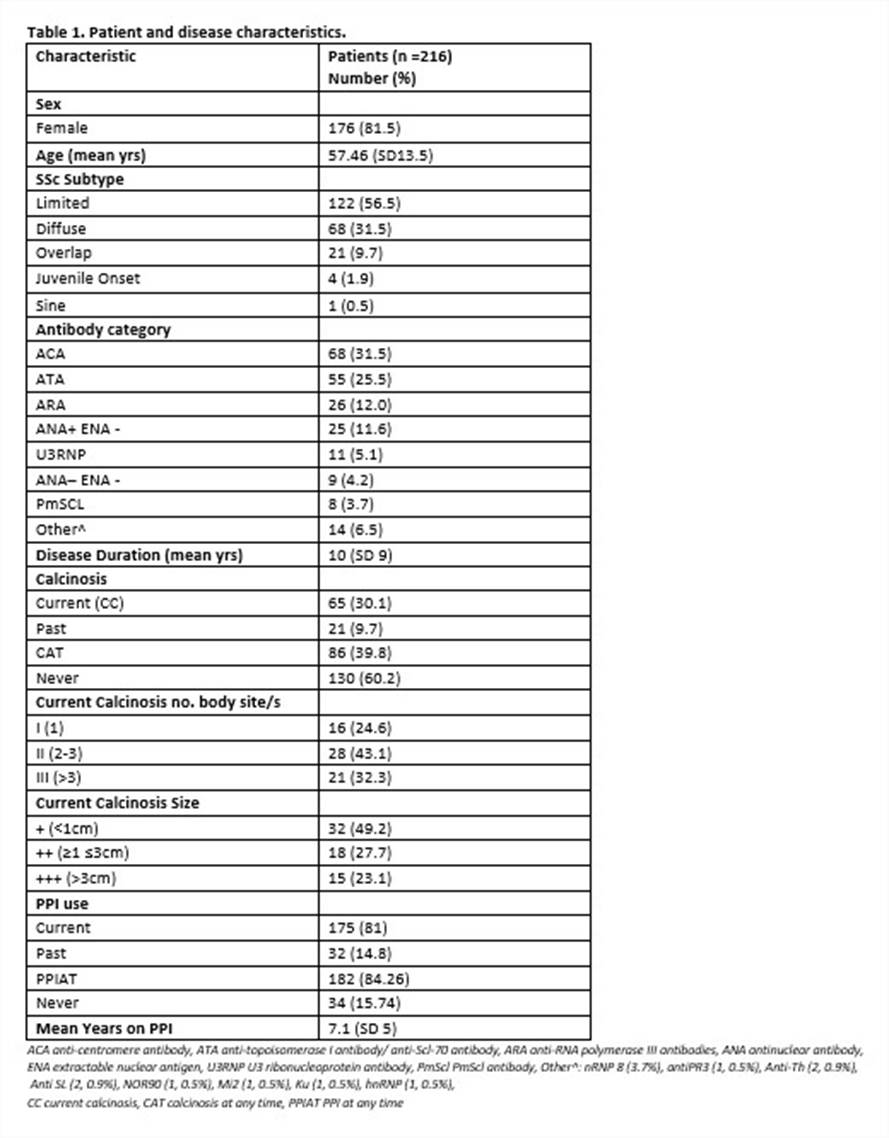
Results: 216 patients were recruited. Table 1 outlines patient and disease characteristics, including calcinosis and PPI use. Gastroesophageal reflux symptoms occurred in 83.3% of patients. Eleven (73.3%) of patients with large volume calcinosis (>3cm) had a PPE for > 10 years and all with calcinosis > 3cm had exposure to PPI. Of patients with only one body site involved 7/16 (43.75%) had PPE category 3 (>10 y). While of those patients with > 1 body site involved 36/49 (73.5%) had a PPE cat >10 years. The most frequent sites for calcinosis were finger (70.8%), elbow (35.4%) and knee (18.5%).
Univariable analysis found associations between calcinosis at any time (CAT) and; disease duration (CAT OR 1.07, CI 1.04-1.11, p <0.001), PPE (CAT OR 1.03, CI 1.01-1.05, p = 0.003) and increasing age (CAT OR 1.02, CI 1.00-1.04, p = 0.043). ATA and ANA positivity was associated with a risk reduction of CAT (ATA OR 0.27, CI 0.12-0.58, p = 0.001, ANA+ OR 0.25, CI 0.09-0.70, p =0.009). Greater than 10 years of exposure to PPI increased the odds of calcinosis by 4 times (CAT OR 4.07, CI 1.68-9.85, p = 0.002) compared to no exposure.
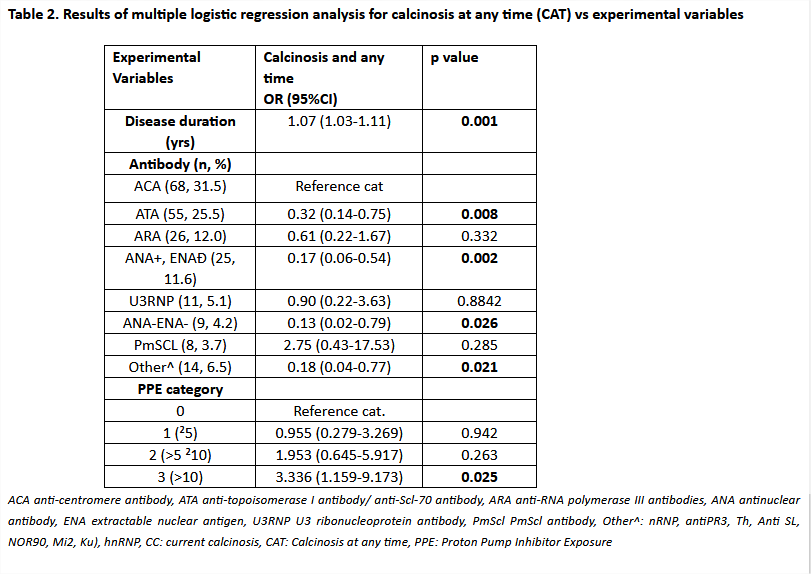
Multivariable logistic regression results are shown in Table 2. Although the effect of PPI on calcinosis was attenuated after adjusting for disease duration and antibodies, higher exposure to PPI remained a significant predictor of calcinosis, with PPE category 3 (>10) increasing risk of CAT (OR 3.34, CI 1.16-9.17, p = 0.025).
Conclusion: We confirm a significant association between PPI exposure with calcinosis in SSc. Given the clinical impact of calcinosis, a potentially modifiable risk factor of PPI exposure warrants further study.
To cite this abstract in AMA style:
Host LV, Campochiaro C, Nihtyanova SI, Denton CP, Ong VH. Prospective Confirmation of Potential Link between Proton Pump Inhibitor Exposure and Calcinosis in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/prospective-confirmation-of-potential-link-between-proton-pump-inhibitor-exposure-and-calcinosis-in-systemic-sclerosis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prospective-confirmation-of-potential-link-between-proton-pump-inhibitor-exposure-and-calcinosis-in-systemic-sclerosis/