Session Information
Date: Tuesday, November 7, 2017
Title: Pediatric Rheumatology – Clinical and Therapeutic Aspects Poster III: Juvenile Arthritis
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with juvenile idiopathic arthritis (JIA) often present with signs and symptoms suggestive of infection. However, it is a diagnostic challenge to differentiate infectious from non-infectious presentation in routine clinical care. Procalcitonin (PCT) is a serum biomarker elevated in the setting of bacterial infection, but whether it can reliably differentiate infection from disease flare in patients with JIA is unknown.[1] We conducted a prospective cohort study to test the hypothesis that PCT levels will differ between active JIA, quiescent JIA, bacteremic patients and healthy controls.
Methods: From 10/16-4/17, consecutive children 6 months – 18 years with a) active untreated JIA (=>4 inflamed joints) b) quiescent JIA and c) healthy elective pre-surgical candidates were recruited from clinics at a musculoskeletal specialty hospital. JIA was defined according to ILAR criteria. Patients with active JIA despite treatment were excluded, to avoid confounding by treatment. Consecutive bacteremic patients were identified from an associated pediatric intensive care unit over the same period. No matching was performed. PCT as well as other common measures of inflammation were compared. Descriptive statistics and univariate logistic analyses were performed as appropriate. The study was IRB approved.
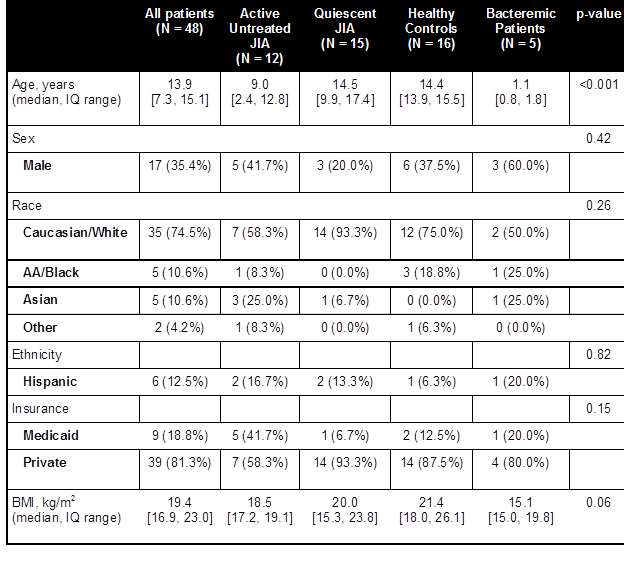
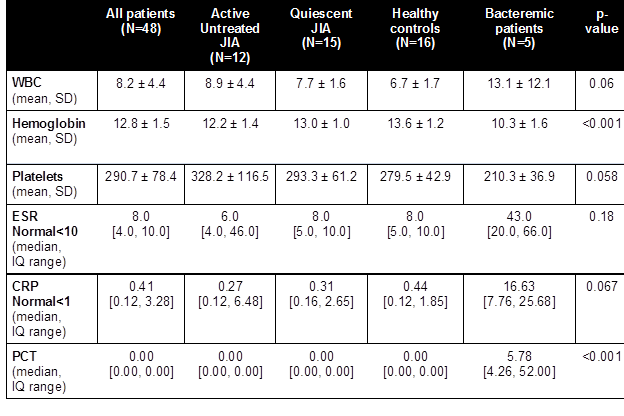
Results: Patient characteristics are summarized in Table 1. Bacteremic patients were younger (mean age 1.1 vs. 14.1 years) and had Staphylococcus aureus (80%) and Kingella kingae (20%) infections. PCT was elevated in bacteremic patients, and was undetectable in all other subjects (p-value <0.001; Table 2). There were trends towards higher ESR and CRP in bacteremic patients, but these were not statistically significant.
Conclusion: Serum PCT levels appear to be a reliable biomarker to distinguish infection vs. active JIA at presentation, and can aid in directing therapy. However, PCT does not appear to be a useful biomarker to assess disease activity in JIA. Further studies are needed to assess utility of serum PCT measurement in differentiating JIA flares from less severe infections.
Table 1. Patient characteristics
Table 2. Laboratory data
[1] Karen Milcent et al., “Use of Procalcitonin Assays to Predict Serious Bacterial Infection in Young Febrile Infants,” JAMA Pediatrics 170, no. 1 (January 1, 2016): 62–69, doi:10.1001/jamapediatrics.2015.3210; Abdel Hakeem Abdel Mohsen and Bothina Ahmed Kamel, “Predictive Values for Procalcitonin in the Diagnosis of Neonatal Sepsis,” Electronic Physician 7, no. 4 (August 2015): 1190–95, doi:10.14661/2015.1190-1195.
To cite this abstract in AMA style:
Trachtman R, Murray ET, Pan N, Toussi SS, Nellis ME, Szymonifka J, Taber S, Adams A, Lehman TJA, Onel K, Mandl LA. Procalcitonin Differentiates Infection from Active Disease in Patients with Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/procalcitonin-differentiates-infection-from-active-disease-in-patients-with-juvenile-idiopathic-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/procalcitonin-differentiates-infection-from-active-disease-in-patients-with-juvenile-idiopathic-arthritis/