Session Information
Date: Monday, November 11, 2019
Title: Epidemiology & Public Health Poster II: Spondyloarthritis & Connective Tissue Disease
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Probiotics have been hypothesized to mediate inflammation through gut microbiome modulation, and growing evidence has suggested that our intestinal gut microbiome may play a role in the development or persistence of spondyloarthritis. This has become understood to some degree among patients who frequently ask about the possible role of probiotics in PsA. The objective of this study was to evaluate associations between probiotic use and patient-reported outcomes in patients with psoriatic arthritis (PsA).
Methods: We examined probiotic use among patients with PsA in FORWARD, The National Databank for Rheumatic Diseases. Patients with rheumatoid arthritis (RA) acted as a comparison group, and patients with dual diagnoses were excluded. The prevalence of probiotic use was determined for each calendar year since the earliest report on record in the databank. Patients who reported probiotic use in at least one encounter were classified as probiotic users. For comparisons made between probiotic users and nonusers, we used propensity score matching to balance confounders. Descriptive statistics were calculated for patient demographics, clinical characteristics, and five outcomes of interest (PAS-II, HAQ-II, pain VAS, SF-36 PCS, and SF-36 MCS). Significance was assessed with Student’s t-tests and Fisher’s exact tests as appropriate. Paired t-tests were utilized to assess differences in outcomes before and after probiotic use in the PsA cohort.
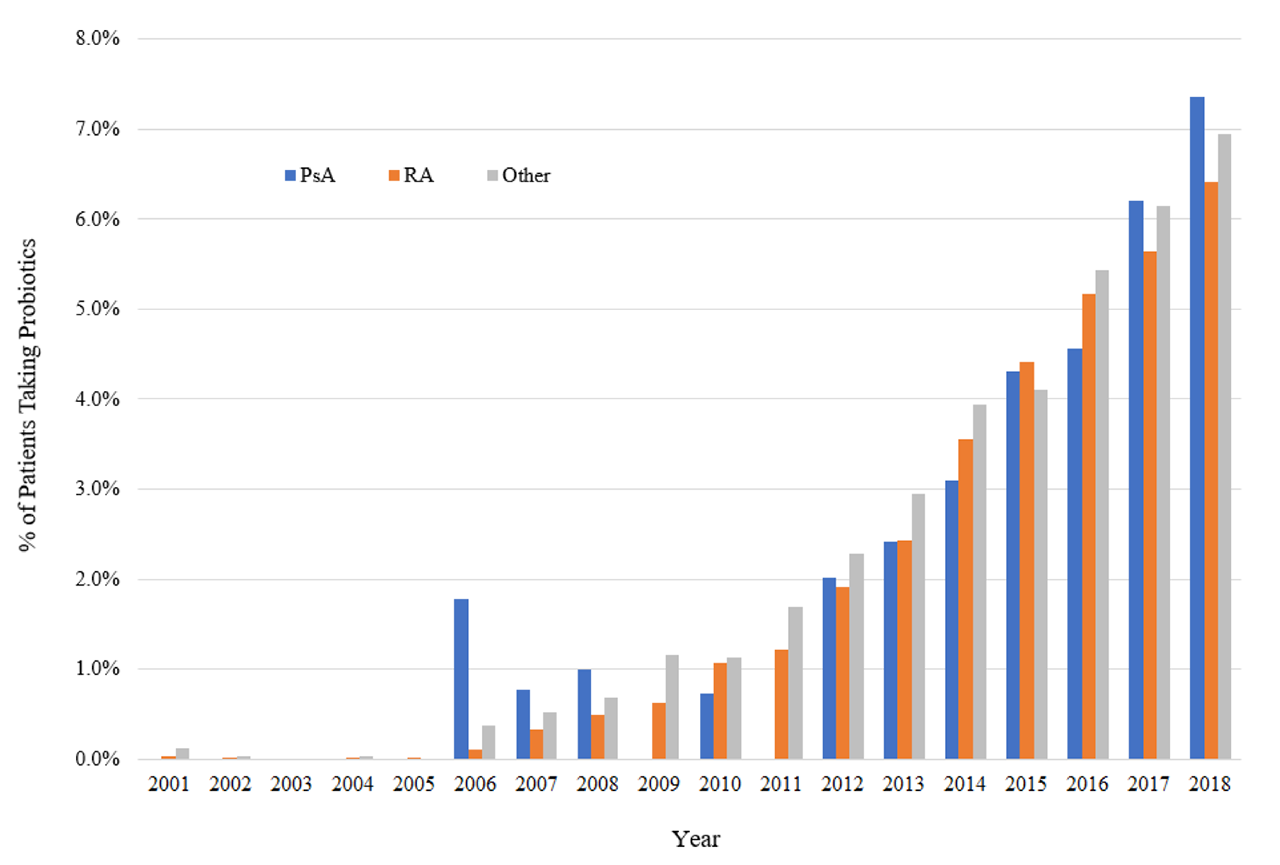
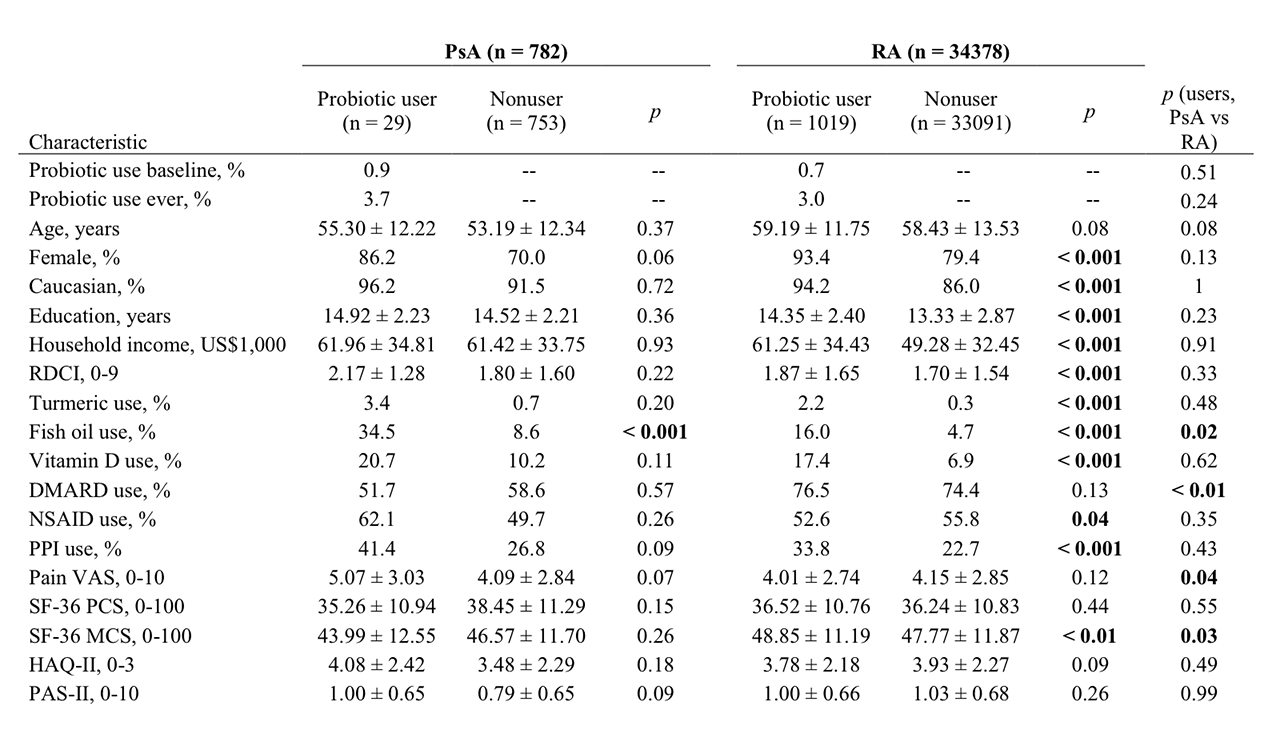
Results: Probiotic use has increased in recent years, from less than 1% prior to 2006 to approximately 7% of FORWARD patients reporting probiotic use in 2018 (Figure 1). Of the 782 PsA and 34,378 RA patients included in the study, 3.7% and 3.0% reported probiotic use at some point, respectively. In the RA cohort, probiotic users are more likely than nonusers to be female, be Caucasian, have more education, have a higher income, have a higher comorbidity index, use PPIs, and use other supplements in addition to probiotics. Probiotic users and nonusers in the PsA cohort generally follow these same trends, but the differences do not reach statistical significance except in the case of fish oil use (Table 1). After propensity score matching, probiotic users with PsA had significantly lower SF-36 PCS scores and significantly higher pain VAS scores than nonusers with PsA (Table 2). In the paired comparison of probiotic users with PsA before initiating probiotic use and after probiotic exposure, there were no statistically significant differences in any of the five outcomes.
Conclusion: We found increasing probiotic use reported by patients with PsA. In this observational study, we found no significant changes in patient function scores before and after initiation of a probiotic. Prospective studies are needed to examine whether probiotics affect disease activity and function in patients with PsA. Given the difference noted in pain scores between probiotic users and nonusers with PsA, patients who take probiotics may have higher baseline pain levels.
To cite this abstract in AMA style:
Grinnell M, Wipfler K, Ogdie A, Michaud K. Probiotic Use and Psoriatic Arthritis Disease Activity [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/probiotic-use-and-psoriatic-arthritis-disease-activity/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/probiotic-use-and-psoriatic-arthritis-disease-activity/