Session Information
Date: Tuesday, November 14, 2023
Title: (2227–2256) Spondyloarthritis Including Psoriatic Arthritis – Treatment: SpA Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: In Psoriatic arthritis (PsA), patients who fail to respond to biologics and targeted synthetic therapies (ts/bDMARDs), switching to another ts/bDMARD should be considered. Failure can be classified as primary non-response (without initial response probably due to therapeutic target failure), or secondary non-response (initial response achieved, but effectiveness is lost over time). Focusing in primary non-response, it seems reasonable to consider a different mode of action for the next treatment rather than switching within class, but studies addressing the best possible strategy are still lacking. Our purpose was obtain information from clinical practice regarding failures due to primary non-responsein PsA on ts/bDMARDs: 1) to assess the incidence rate of switching due to primary non-response; and 2) in those who have experienced primary non-response, to assess the risk of subsequent treatment failure by switching between classes compared to switching within class.
Methods: A longitudinal retrospective study (2015-2022) of PsA patients meeting CASPAR criteria on treatment with ts/bDMARDs from an outpatient rheumatology clinic was conducted. Main outcomes: 1) ts/bDMARD failure due to primary non-response; 2) subsequent discontinuation of ts/bDMARD due to lack of efficacy. Ourindependent variable wasswitching between classes compared to switching within class. To estimate bDMARDs switching rates, survival techniques were used, expressing the incidence rate (IR) per 100 patients*year with their CI at 95%. Cox multivariate regression analyses was run to assessthe role of switching between/within classes in the subsequent treatment failure.
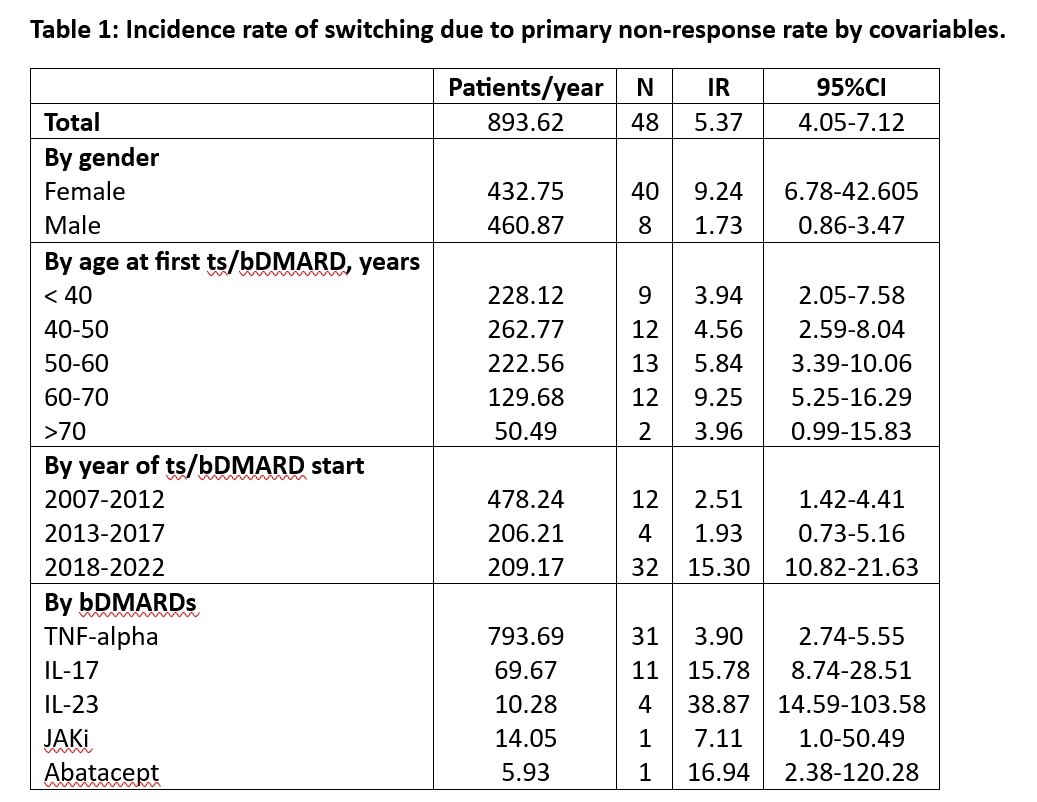
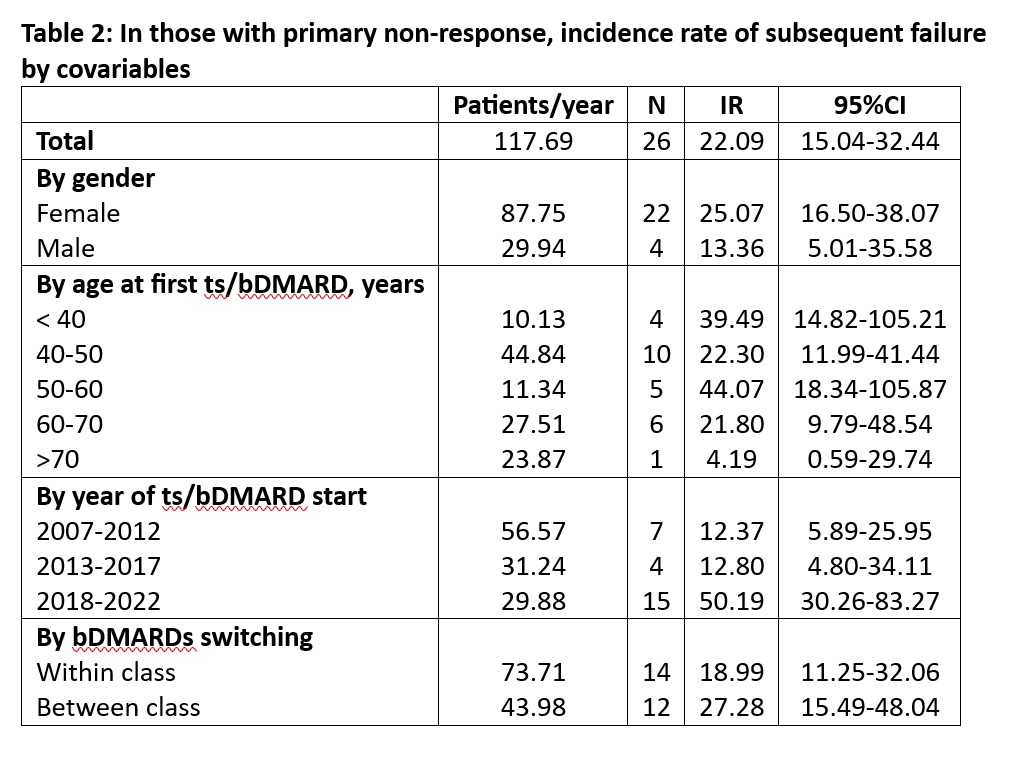
Results: 141 PsA patients on treatment with ts/bDMARDs with a maximum follow-up of 16 years were included. Of these, 30 in 48 treatment courses developed primary non-response with an IR of 5.37 [4.04-7.12]. The IR was higher in women, and in those that started ts/bDMARDs after 2018. Regarding ts/bDMARDs those on TNF developed lower IR compared to the others (Table1). Focusing in those with primary non-response, there were 26 subsequent treatment failures with an IR of 22.09 [15.04-32.44]. The IR was higher in women, mainly after 2018 and in those patients who switched between classes (Table 2). In the multivariate adjusted model we found that switching within class increased the risk of subsequent failure compared switching between class (HR:3.26 [1.23-8.62], p=0.017).
Conclusion: In clinical practice, the IR of ts/bDMARDs failures due to primary non-response is 5.37% patients*year, but their subsequent failures are higher. This study provides a support to consider switching between classes a better alternative rather than switching within class after primary non-response.
To cite this abstract in AMA style:
Abasolo l, Leon L, Rodriguez Laguna M, Toledano E, Candelas G, Martinez C, Alvarez Hernandez M, Fernandez B, Freites D. Primary Non-response in Psoriatic Arthritis Treated with Biologics and Targeted Synthetic Therapies in Daily Clinical Practice [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/primary-non-response-in-psoriatic-arthritis-treated-with-biologics-and-targeted-synthetic-therapies-in-daily-clinical-practice/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/primary-non-response-in-psoriatic-arthritis-treated-with-biologics-and-targeted-synthetic-therapies-in-daily-clinical-practice/