Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The extraintestinal manifestations of Inflammatory Bowel Disease (IBD) are identified in 6%-40% of patients. Systemic vasculitides may present as extraintestinal manifestations of IBD. The purpose of this study was to determine the frequency of vasculitides (large, medium or small vessel) in a cohort of patients with IBD.
Methods: This is a retrospective chart review of patients from 12/2006 to 12/2016 at a single tertiary medical center. A cohort of patients with diagnosis codes for inflammatory bowel disease including Crohn’s disease (CD), Ulcerative colitis (UC) and Microscopic colitis (MC) was identified. Patients with vasculitides including giant cell arteritis (GCA), Takayasu’s arteritis (TA), PAN, aortitis, ANCA associated vasculitis, GPA, MPA, EGPA, CNS vasculitis, cryoglobulinemic vasculitis, cutaneous vasculitis, Leukocytoclastic vasculitis (LCV), Pulmonary vasculitis, Rheumatoid vasculitis, small vessel vasculitis (SVV), and retinal vasculitis were identified. One sided student’s t-tests were used for statistical analysis.
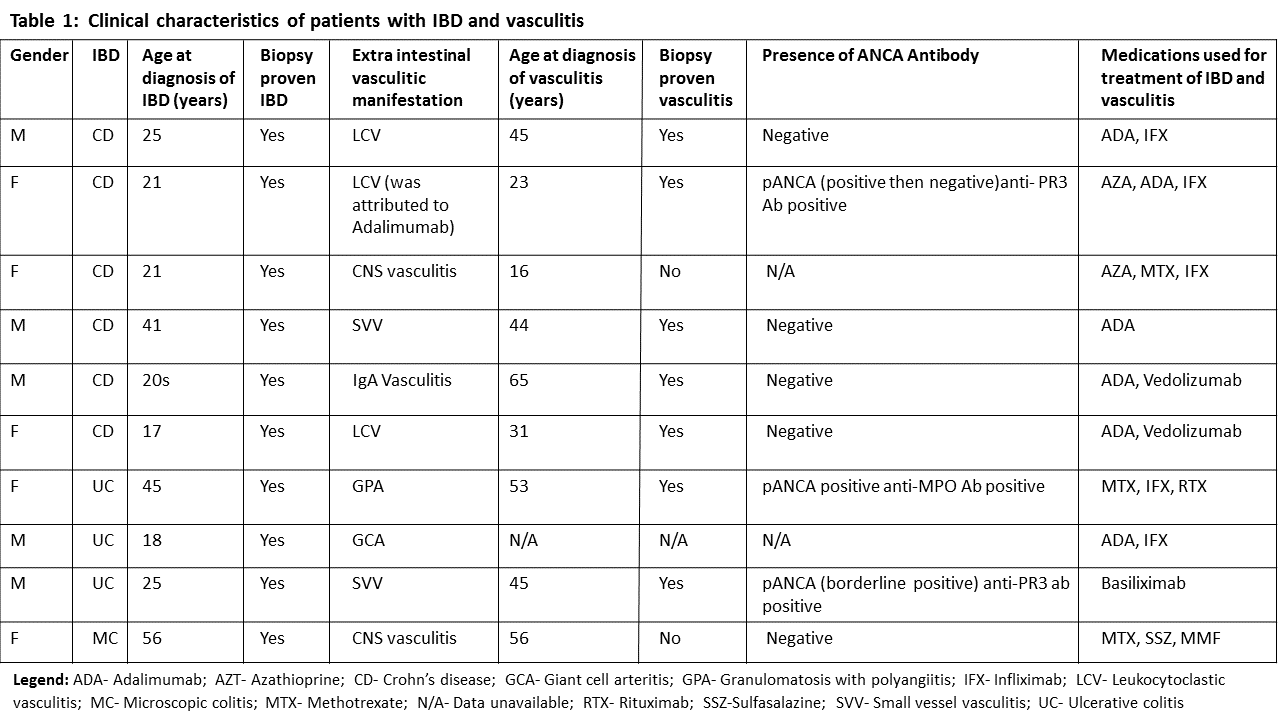
Results: An EMR query yielded a total of 1686 patients, of whom 913 patients were diagnosed with CD, 695 with UC and 78 with MC. A search for a concomitant diagnosis code for vasculitis yielded 10 patients (10/1687=0.59%). Of the 10 patients, 6 had CD (60%), 3 had UC (30%) and 1 had MC (10%). Both genders had equal representation. The mean age at diagnosis of IBD was 29.4 years with males being diagnosed at a younger age; 26.8 vs 32 years (p=0.28). Vasculitis presented later, at a mean age of 42. The difference in the age at diagnosis of IBD and vasculitis was statistically significant overall (12.6 years; p=0.038). The most common extraintestinal manifestation of vasculitis was LCV (3, 30%) followed by SVV (2, 20%) and CNS vasculitis (2, 20%). Immunological evaluation did not reveal increased incidence of ANCA antibodies (table 1). Only 3 patients (30%) were ANCA positive, 5 were ANCA negative and data was missing for 2 patients. In this cohort of patients with IBD about 0.6% developed vasculitis with an estimated prevalence of extraintestinal manifestations of vasculitis of 590 per 100,000 which is higher compared to reported prevalence rates of vasculitides such as GPA and GCA which has which have a prevalence of 13.5 and 278 per 100,000 based on population studies in the UK and Minnesota, USA respectively.
Conclusion: In this cohort of patients with IBD, a small percentage of patients developed vasculitis. However, in the majority of cases vasculitis was diagnosed after the onset of IBD suggesting that vasculitis may be secondary to IBD or IBD-related treatments.
To cite this abstract in AMA style:
Ifteqar S, Springer J, Maz M. Prevalence of Vasculitides As Extraintestinal Manifestation of Inflammatory Bowel Disease (IBD) [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-vasculitides-as-extraintestinal-manifestation-of-inflammatory-bowel-disease-ibd/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-vasculitides-as-extraintestinal-manifestation-of-inflammatory-bowel-disease-ibd/