Session Information
Date: Tuesday, November 12, 2019
Title: Epidemiology & Public Health Poster III: OA, Gout, & Other Diseases
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Thyroid dysfunction (TD) is known as a common complication of rheumatological diseases (RD). Treatment for TD is important not only in clinical TD for controlling symptom but also in some patients with subclinical ones especially for cardiovascular events in the future. But the data about prevalence of hypothyroidism or hyperthyroidism requiring treatment and it’s changes with follow up in patients with RD is limited.
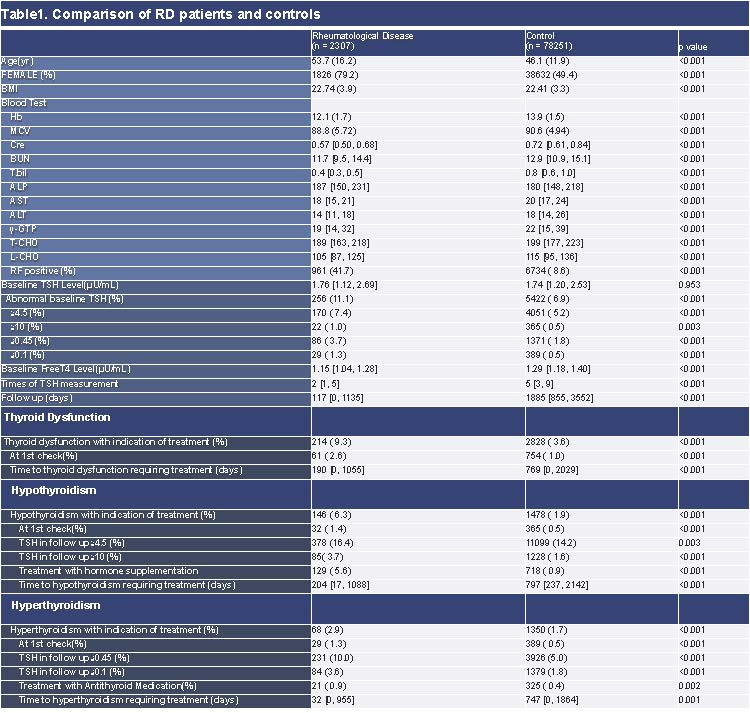
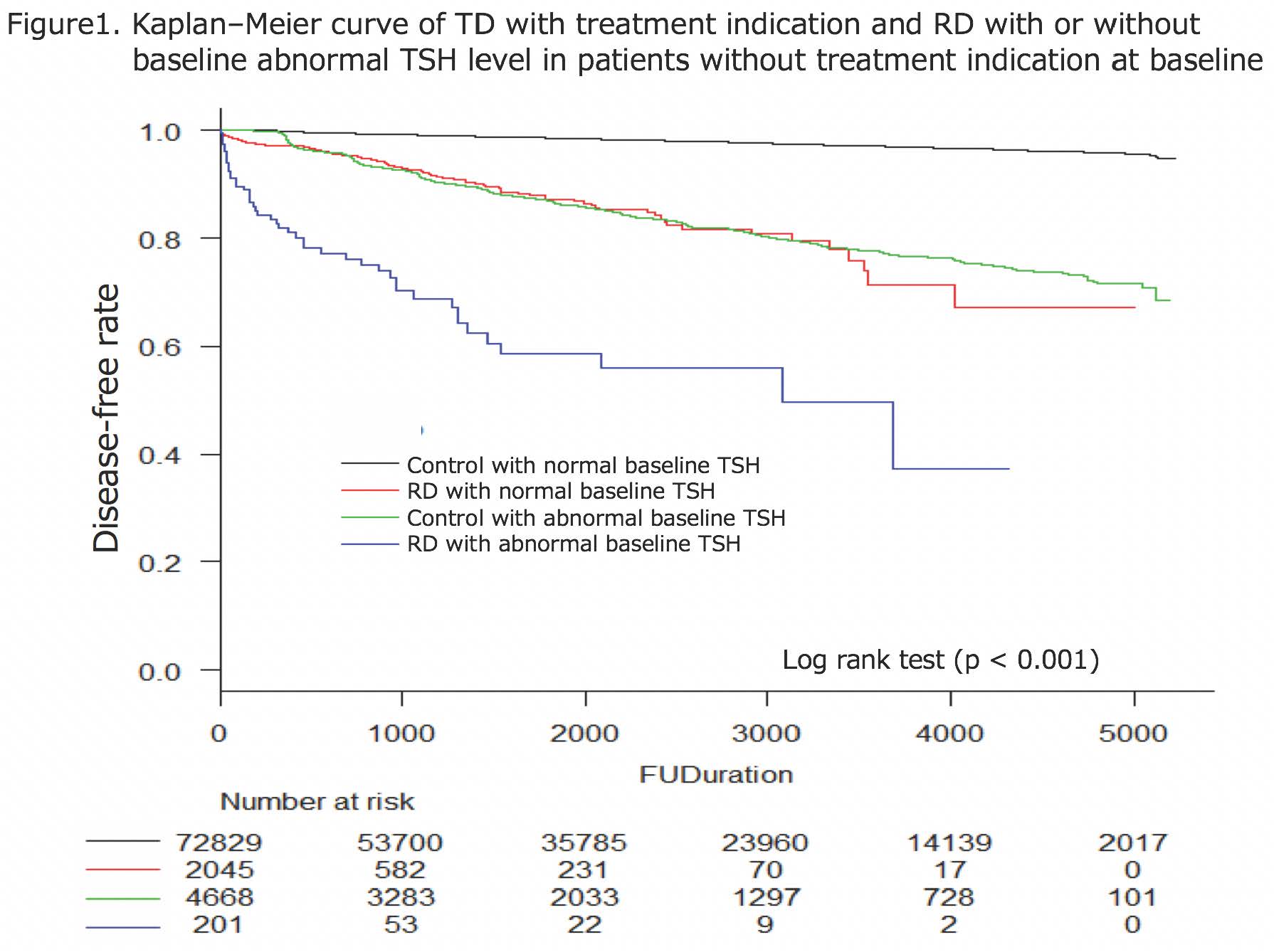
Methods: We retrospectively reviewed charts of consecutive patients with RD and healthy controls who checked TSH (thyroid stimulating hormone) level at least once at immuno-rheumatology center and preventive medicine center, in St. Luke’s International Hospital, Tokyo, Japan, from January 2004 to July 2018. We investigated basic demographics, underlying diseases, blood tests including thyroid functions and treatment with thyroid hormone or antithyroid medications. We compared the number of TD requiring treatment (TSH ≧10 μU/mL, TSH ≦0.1 μU/mL or physician started treatment) and it’s changes in follow up using univariate analysis and Kaplan–Meier method with log rank test. The risk of TD which needs treatments was assessed with Cox proportional hazard model in all subjects and logistic regression analysis in RD patients.
Results: 2307 RD patients and 78251 controls without past medical history of TD requiring treatments are included. Newly-detected TD requiring treatments are significantly frequent in RD patients (214, 9.3% vs 2828, 3.6%, P< 0.001). When focused on patients without TD requiring treatment at baseline, Kaplan–Meier method and Cox’s proportional hazards model revealed hazard ratio of TD with indication of treatment is significantly higher in RD patients with baseline abnormal TSH(≦0.45 or ≧4.5 μU/mL) (HR=32.6; 95%CI 24.3-43.9, p< 0.001), RD with normal baseline TSH (HR=7.5; 95%CI 6.1-9.2, p< 0.001), control with abnormal TSH (HR=8.5; 95%CI 7.8-9.3, p< 0.001) when compared to controls with normal TSH at baseline after adjusting confounders. When focus on RD patients, female, patients with ANA(anti-nuclear antibody) related disease, baseline abnormal TSH level, and positive thyroid-related antibodies at baseline have statistically significant higher risk of TD requiring treatment after adjusting confounders in multivariate analysis.
Conclusion: TD with therapeutic indication are much more frequent in RD patients, especially with abnormal baseline TSH level, and about 1 out of 10 RD patients has TD requiring treatment. We encourage active routine measurement of thyroid function tests in RD patients especially with above risk factors.
To cite this abstract in AMA style:
Fukui S, Kidoguchi G, Nakai T, Kawaai S, Ozawa H, Koido A, Ikeda Y, Suda M, Yanaoka H, Shimizu H, Tamaki H, Tsuda T, Kishimoto M, Yamaguchi K, Okada M. Prevalence of Thyroid Dysfunction with Therapeutic Indication in Patients with Rheumatological Diseases [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-thyroid-dysfunction-with-therapeutic-indication-in-patients-with-rheumatological-diseases/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-thyroid-dysfunction-with-therapeutic-indication-in-patients-with-rheumatological-diseases/