Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Saturday, May 2, 2020
Title: Poster Session 3
Session Type: ACR Abstract Session
Session Time: 4:15PM-5:15PM
Background/Purpose: Paradoxical psoriasis after exposure to tumor necrosis factor inhibitors (TNFi) has been increasingly reported in the adult population. Systematic studies in pediatric population are lacking. Most case series that are available describe the disease course of psoriasis. Recently the relative risk of psoriasis was shown to be increased in children with inflammatory bowel disease (IBD), and juvenile idiopathic arthritis (JIA) after exposure to TNFi but not in children with chronic nonbacterial osteomyelitis (CNO). We aimed to investigate the relationship between TNFi therapy and the onset of new, or exacerbation of existing, psoriasis in children.
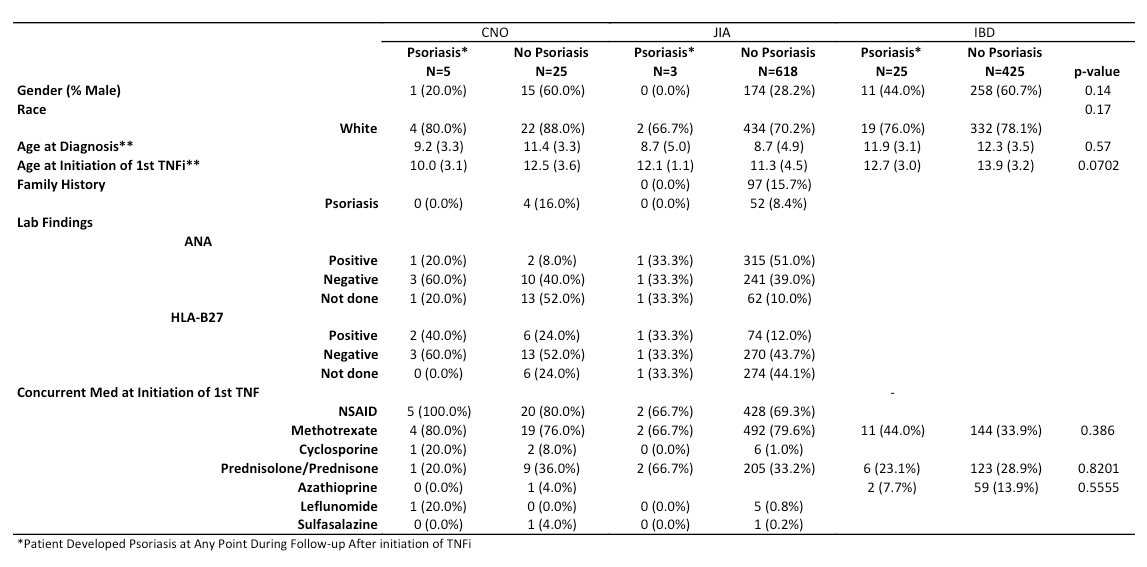
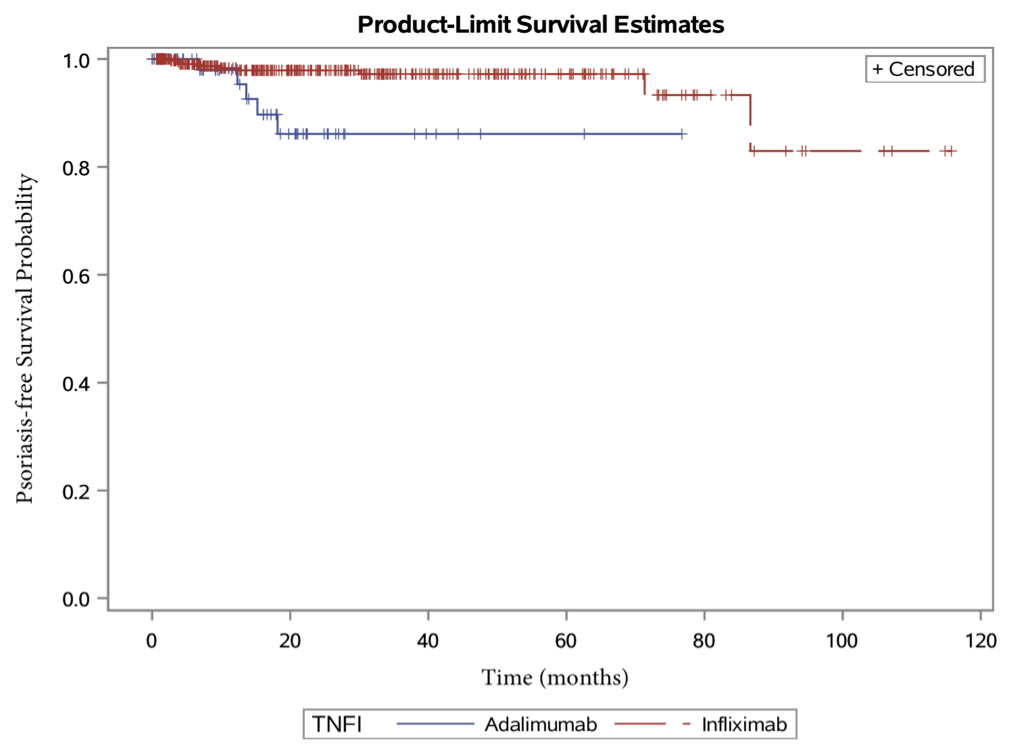
Methods: Identification of patients with diagnosis of CNO, JIA, IBD or psoriasis was performed by querying the electronic medical database using standard ICD-9 codes. Inclusion criteria were: (a) children were younger than 18 years old at the diagnosis of CNO, JIA, or IBD; (b) children were seen at least twice at the rheumatology or gastroenterology clinic at Seattle Children’s Hospital between January 1st, 2005 and July 31st, 2015; and (c) children were treated with TNFi during the observational window. Clinical and demographic characteristics were summarized descriptively by disease type (CNO, JIA, IBD) as well as psoriasis status. Baseline characteristics were compared among those developing psoriasis vs. those who did not using t-tests or Wilcoxon Rank Sum tests. Kaplan-Meier curves are used to show psoriasis-free survival time after initiation of prescribed TNFi overall, as well as, by specific TNFi type among IBD patients.
Results: A total of 1,091 patients were included. Median follow up time from initiation of first TNFi was 20.7 months for CNO patients, 35.8 months for JIA patients and 36.1 months IBD patients. Psoriasis developed or worsened after exposure to TNFi in 5 of 30 CNO patients (17%), 3 of 621 JIA patients (0.5%) and 25 of 450 IBD patients (6%). There was no significant difference in distribution of age, gender, family history or concomitant medications between psoriasis subset and no psoriasis subset as shown in Table 1. Among various TNFi, adalimumab and infliximab were more commonly associated with psoriasis. Within IBD group, adalimumab was associated with earlier onset of psoriasis than infliximab (p< 0.004, Figure 1). Among those who developed psoriasis, 88% had plaque psoriasis, 25% with alopecia and 84% with scalp psoriasis. 38% had partial and 47% had complete responses to topical or phototherapy. Fourteen patients (44%) discontinued or switched therapies.
Conclusion: TNF inhibitor-induced psoriasis is more common in patients with CNO and IBD than JIA. Within IBD cohort, adalimumab is more likely to induce psoriasis than infliximab. Majority of patients had favorable outcomes to topical treatments and phototherapy. Patients and family need to be educated about the risk of developing psoriasis prior to initiation of TNFi.
To cite this abstract in AMA style:
Kodama S, Gupta D, Sullivan E, Zhao Y. Prevalence of Paradoxical Psoriasis After Exposure to Tumor Necrosis Factor Inhibitors (TNFi) in Children from a Single Tertiary Center [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/prevalence-of-paradoxical-psoriasis-after-exposure-to-tumor-necrosis-factor-inhibitors-tnfi-in-children-from-a-single-tertiary-center/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-paradoxical-psoriasis-after-exposure-to-tumor-necrosis-factor-inhibitors-tnfi-in-children-from-a-single-tertiary-center/