Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Autoinflammatory diseases (AIDs), often caused by single gene mutations, are disorders in which aberrant activation of innate immune cells causes uncontrolled systemic inflammation. Because many autoinflammatory mediators negatively regulate of allergic/atopic cytokines, patients with AIDs are thought to be at low risk of developing atopy. However, the prevalence of atopy in the AIDs is not established.
Methods: We conducted a retrospective chart review of patients enrolled on protocol 94-HG-0105 “Genetics and Pathophysiology of Familial Mediterranean Fever and Related Disorders”. All patients had a molecular diagnosis (Sanger sequencing) of familial Mediterranean fever (FMF); cryopyrin-associated periodic syndrome (CAPS); tumor necrosis factor-associated periodic syndrome (TRAPS); deficiency of adenosine deaminase 2 (DADA2), hyper-IgD syndrome (HIDS); pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA); or haploinsufficiency of A20 (HA20). Atopic features were defined as serum IgE > 100 kU/L, absolute eosinophil count (AEC) > 500, true (non-neutrophilic) urticaria, asthma, atopic dermatitis, or food allergy. Severe atopic features were defined as serum IgE > 500, AEC > 1500, anaphylaxis (excluding medication-induced), recurrent angioedema, multiple food allergies, or eosinophilic gastrointestinal disease (EGID). Comparator laboratory data (IgE, AEC) were obtained from theNational Health and Nutrition Examination Survey (NHANES). Comparator data on food allergy, asthma, atopic dermatitis, angioedema, anaphylaxis, and EGID were obtained from US population-based studies (National Health Interview Survey, Behavioral Risk Factor Surveillance System, National Opinion Research Center, US commercial healthcare databases). Comparator data on urticaria and angioedema, which had not been studied in US populations, were obtained from European population-based studies (surveys and national registries).
Results: Atopic features are shown in Table 1, and severe atopic features are shown in Table 2. Clinical features of atopy were less prevalent in AIDs than in the general population except for asthma, which was observed in CAPS, PAPA, and HA20. Of the AIDs, FMF, TRAPS, and HIDS had the lowest prevalence of atopy. With regards to lab features of atopy, AIDs had a low prevalence of elevated IgE, whereas mild eosinophilia was highly prevalent in CAPS, PAPA, and HA20. Severe atopy was rare in all the AIDs, with rates lower than those seen in the general population for all features except eosinophilia. Severe eosinophilia (AEC > 1500) was seen in CAPS and PAPA, and EGID was a prominent component of intestinal inflammation in one HA20 patient.
Conclusion: Most clinical features associated with atopy are rare in AIDs, as is elevated IgE, and the presence of severe atopy in an AID should prompt further investigation. However, both mild and severe eosinophilia are seen at a higher prevalence in CAPS, PAPA, and HA20, suggesting that NLRP3, PSTPIP1, and TNFAIP3mutations may alter eosinophil biology. Further studies are needed to determine the significance, disease associations, and treatment associations of eosinophilia in these diseases.
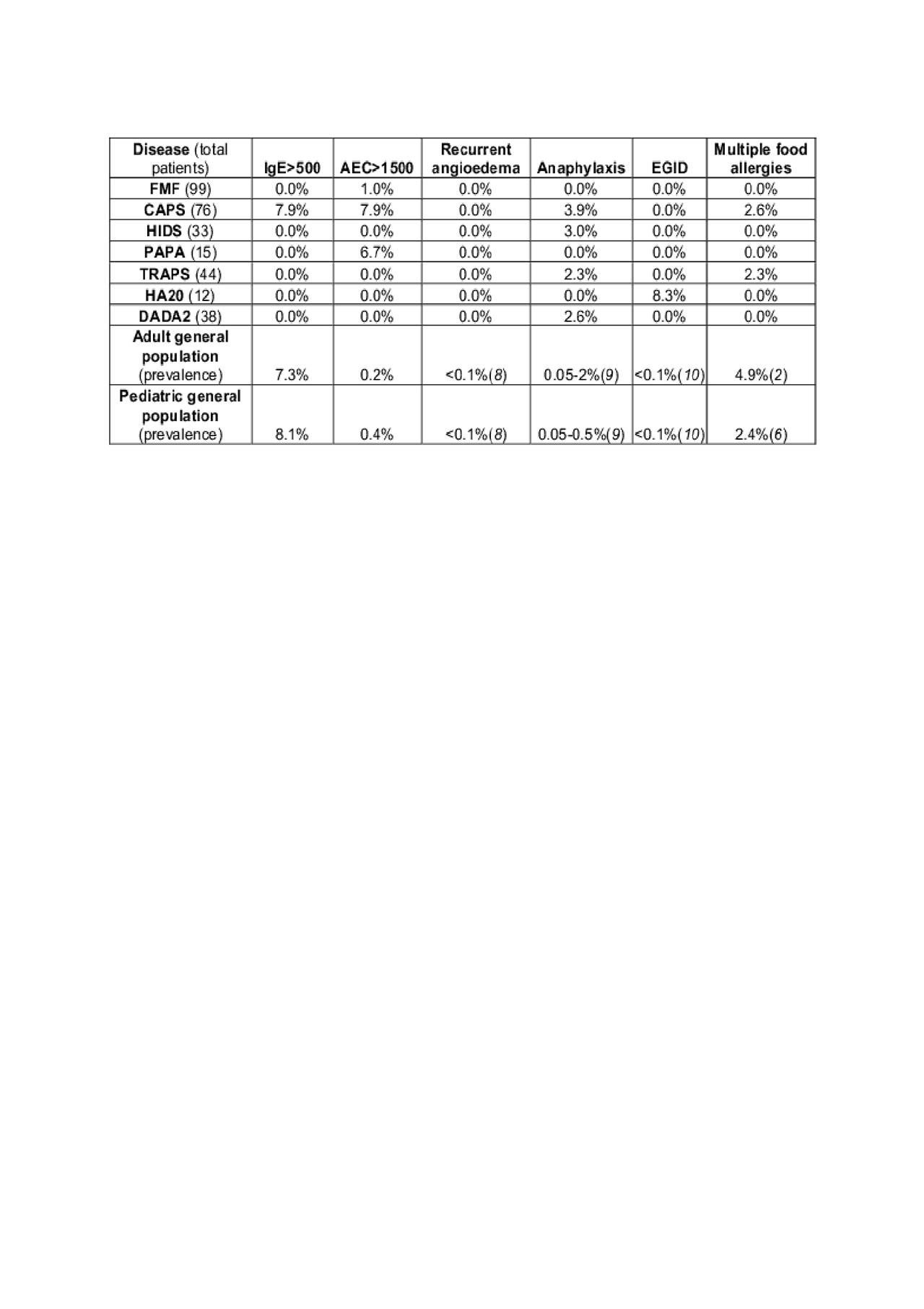
06032019 ACR ABSTRACT TABLE 2 FINAL
References:
1. Aygoren-Pursun E, Magerl M, Maetzel A, Maurer M: Epidemiology of Bradykinin-mediated angioedema: a systematic investigation of epidemiological studies. Orphanet J Rare Dis 2018, 13-1-:73.
2. Yu JE, Lin RY: The Epidemiology of Anaphylaxis. Clin Rev Allergy Immunol 2018, 54-3-:366-374.
3. Mansoor E, Saleh MA, Cooper GS: Prevalence of Eosinophilic Gastroenteritis and Colitis in a Population-Based Study, From 2012 to 2017. Clin Gastroenterol Hepatol 2017, 15-11-:1733-1741.
4. Gupta RS, Warren CM, Smith BM, Jiang J, Blumenstock JA, Davis MM, Schleimer RP, Nadeau KC: Prevalence and Severity of Food Allergies Among US Adults. JAMA Netw Open 2019, 2-1-:e185630.
5. Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, Holl JL: The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics 2011, 128-1-:e9-17.
To cite this abstract in AMA style:
Dizon B, komarow H, Stone D, Hoffmann P, Jones A, Romeo T, Barron K, Aksentijevich I, Kastner D, Ombrello A, Milner J, Schwartz D. Prevalence of Atopic Features in Classic Autoinflammatory Diseases [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-atopic-features-in-classic-autoinflammatory-diseases/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-atopic-features-in-classic-autoinflammatory-diseases/
