Session Information
Date: Saturday, November 6, 2021
Title: Spondyloarthritis Including PsA – Basic Science Poster (0046–0068)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Spondyloarthritis (SpA) encompasses Ankylosing Spondylitis (AS), Psoriatic Arthritis (PsA), Inflammatory bowel disease- associated spondyloarthritis (IBD-SpA), Reactive Arthritis (ReA), and undifferentiated spondyloarthritis. These conditions share a number of extra musculoskeletal manifestations, the most common being acute anterior uveitis.
To determine the frequency and characteristics of SpA associated uveitis, to elucidate associated clinical features of SpA in patients with uveitis, and to identify SpA features that can predict flares of uveitis (UV).
Uveitis occurs more commonly in axial SpA (axSpA) than in PsA
Methods: Patients followed in the axSpA and PsA clinics at a single centre from January 2004 to December 2020 at 6–12-month intervals, according to a standard protocol including demographic and clinical variables, treatment and acute phase reactants.
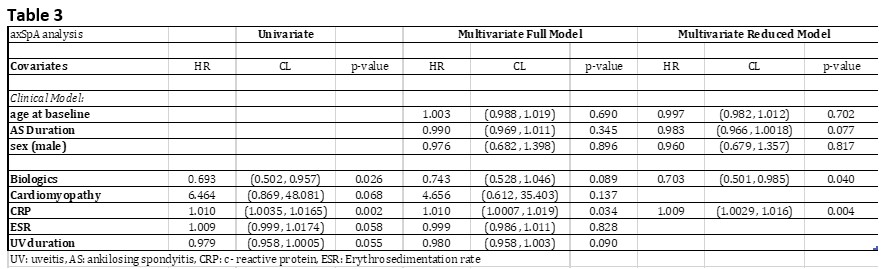
T and chi-squared tests were performed at baseline visits on demographic and clinical factors on both the SpA and PsA populations, to compare patients with and without UV. Cox proportional-hazard models with time-dependent covariates were performed on patients with UV, with their first instance of a UV flare as the outcome event. Univariate analysis was done for each clinical and demographic factor, controlling for age, sex, and disease duration. Factors significant (< 0.1) in the univariate analysis were included in a multivariate analysis, controlling for age, sex and disease duration.
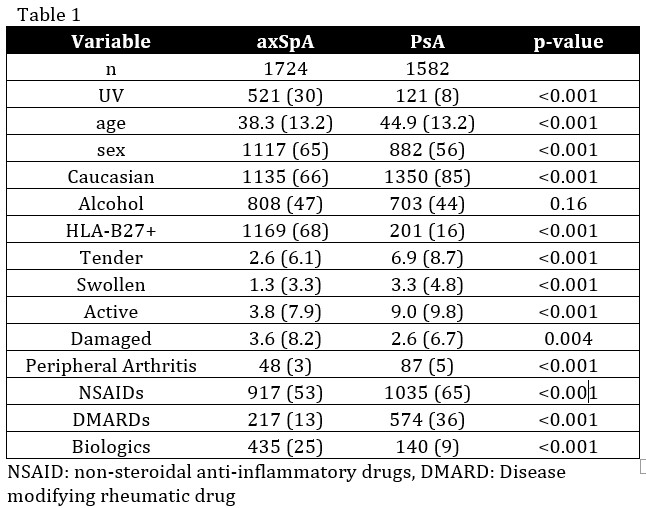
Results: A total of 3306 patients were included, 1724 patients with axSpA and 1582 patients with PsA. 30.2% of the axSpA cohort having uveitis (UV), vs 7.6% in the PsA. The rate of flares per person years at risk was 12.12% in the axSpA cohort, vs 1.71% in the PsA.
Demographic and clinical features are depicted in Table 1. There were more men in the total cohort (axSpA 65% and PsA 56%). More men with UV in the axSpA cohort (65% compared to 47% in the PsA). Most patients were Caucasian (axSpA 67%, 94% PsA)
Among axSpA patients 1169 (68%) were HLA*B27+, and 435 had UV. Among PsA patients 201 (16%) patients were HLA*B27+, and 32 had UV.
The multivariate analysis of the axSpA cohort showed that higher CRP (HR 1.009 p=0.004) increased the risk of a flare, while biologic agents decrease risk of flare (HR 0.702 p=0.040) in patients with UV. In the PsA cohort, being HLA*B27+ (HR 3.084 p=0.007) increased the risk of a UV flare, while being on a DMARD decreased the risk of a flare in patients with UV (HR 0.262 p=0.0088)
Conclusion: The results confirm the hypothesis that uveitis is more common in the axSpA than in the PsA population. New onset of UVs was also more commonly seen in the axSpA cohort. Factors that increase the risk of new uveitis flare were elevated ESR and CRP in the axSpA cohort and being a male or HLA-B27+ in the PsA population.
To cite this abstract in AMA style:
Ocampo V, Sutton M, Ramkissoon S, Kaplan A, Haroon N, Gladman D. Prevalence, Incidence and Predictor Features of Uveitis in Spondyloarthritis in a Canadian Cohort [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/prevalence-incidence-and-predictor-features-of-uveitis-in-spondyloarthritis-in-a-canadian-cohort/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-incidence-and-predictor-features-of-uveitis-in-spondyloarthritis-in-a-canadian-cohort/