Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Polypharmacy is associated with an increased risk of adverse drug effects and medication nonadherence. However, the prevalence of polypharmacy and the medications and factors that contribute to polypharmacy in SLE remain understudied. Our objectives were to estimate the prevalence and correlates of, and identify medications associated with, polypharmacy among individuals with SLE.
Methods: Participants were recruited from a population-based, metropolitan Atlanta cohort [Georgians Organized Against Lupus (GOAL)] of individuals with validated SLE. During a one-time study visit (10/2019-5/2022), prescribed medications were self-reported via survey. Consistent with studies in other populations, we defined polypharmacy and hyperpolypharmacy as >5 and >10 medications, respectively, and calculated the crude prevalence of each. Multivariable regression including sociodemographics (age, sex, race, education, income) and SLE-related variables (disease activity and cumulative disease damage) was used to obtain the adjusted prevalence of polypharmacy by participant characteristics. We also categorized individual medications into relevant groups and calculated the crude prevalence of each medication category by polypharmacy status.
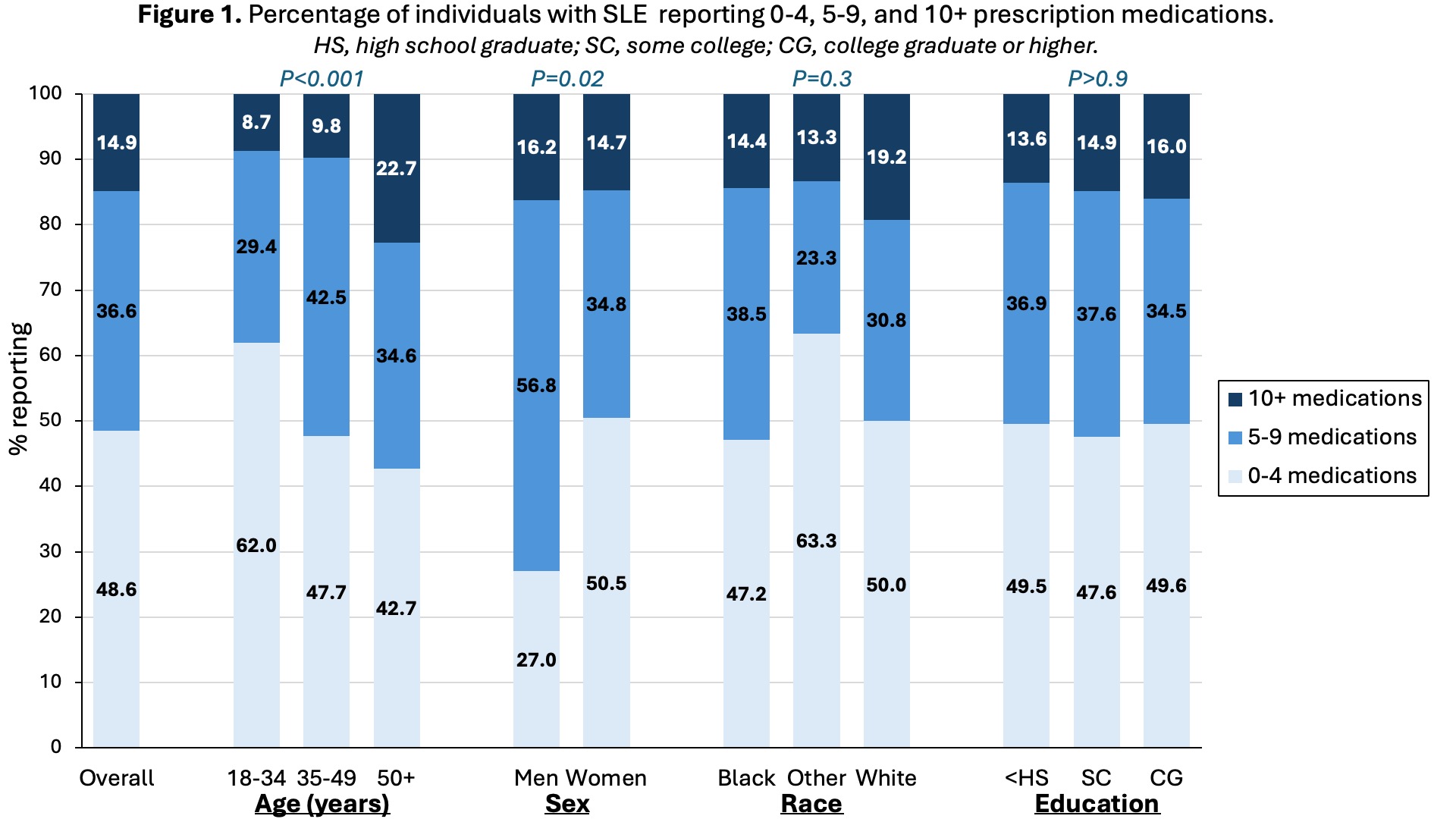
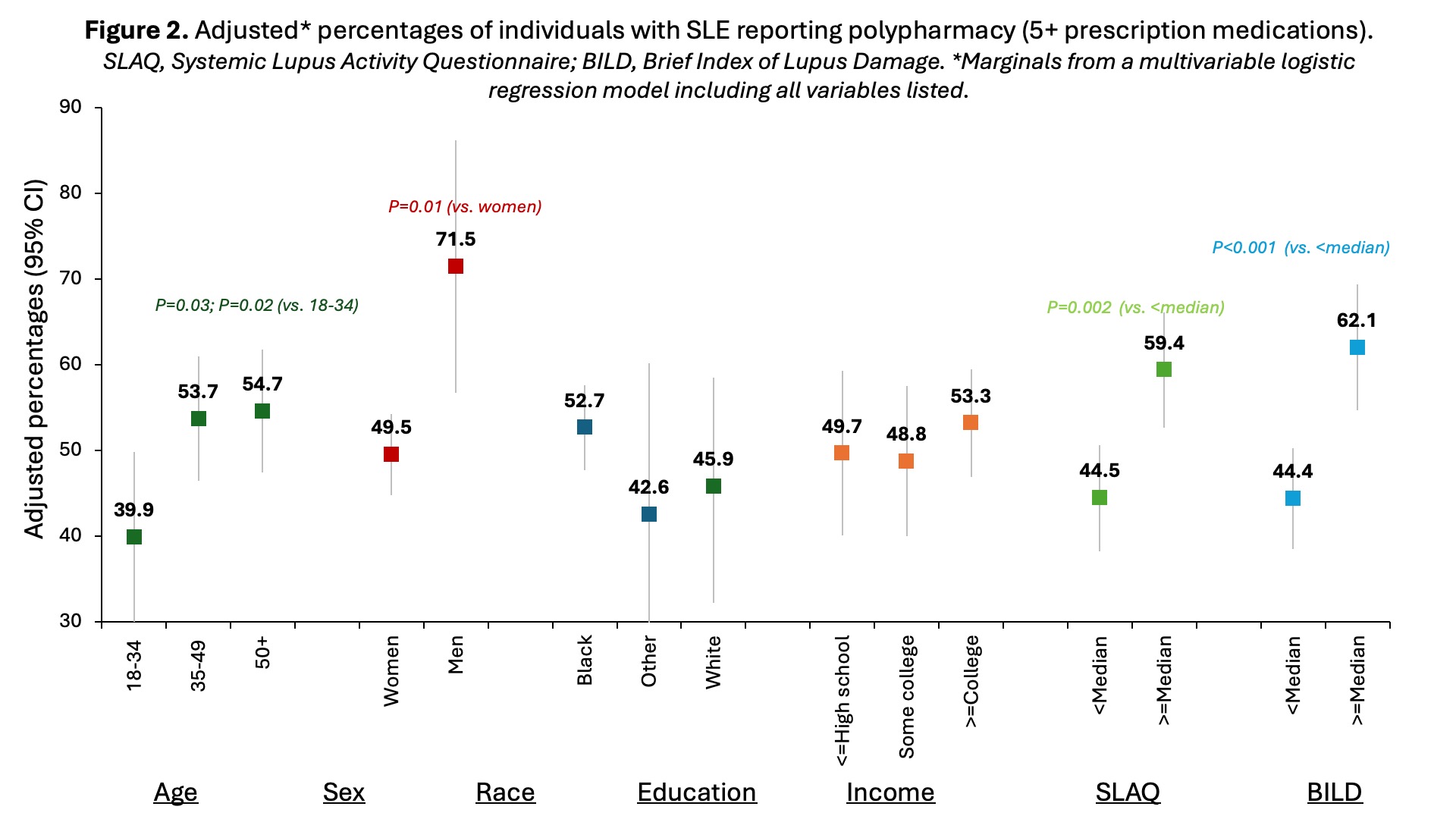
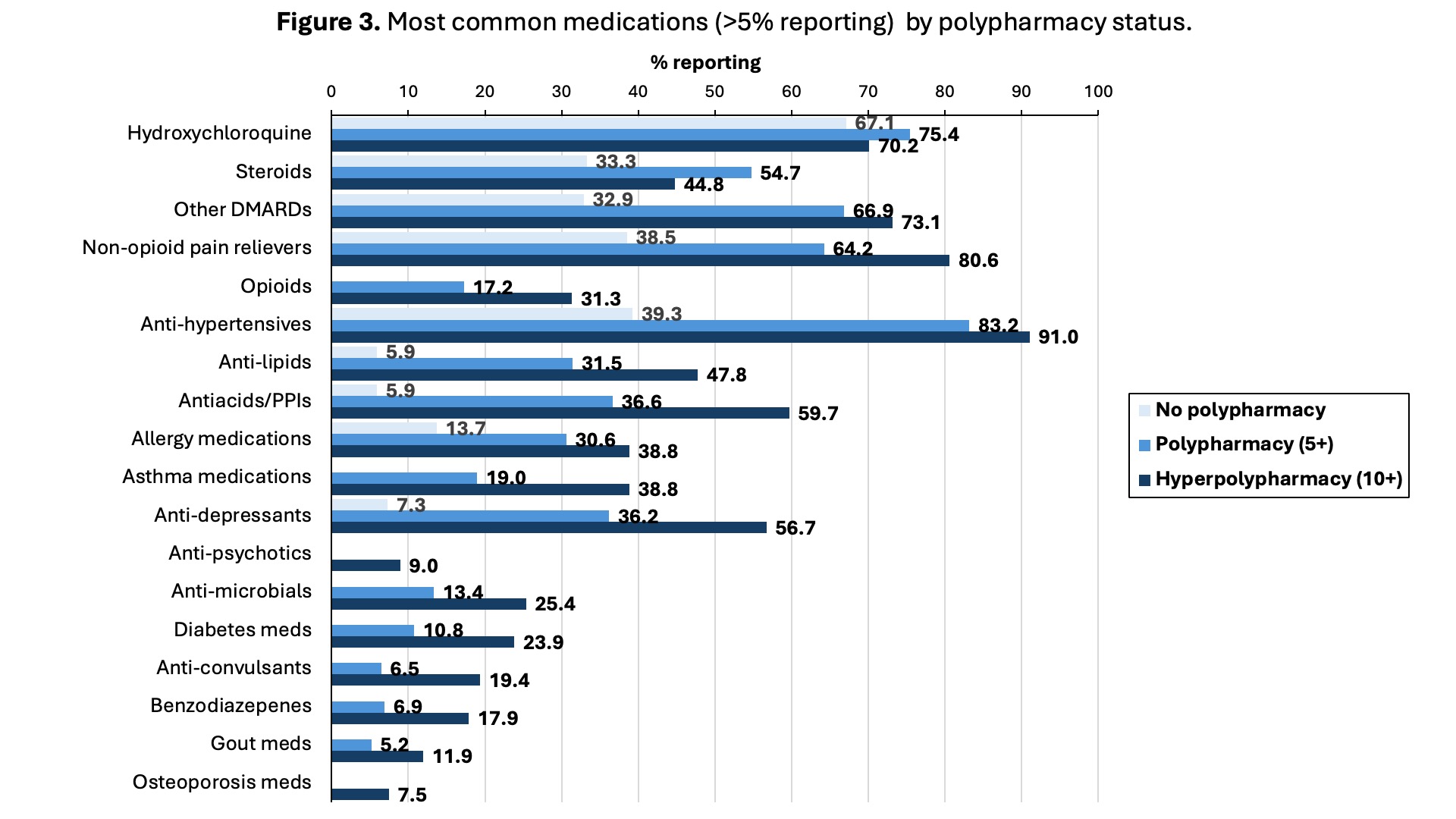
Results: Overall, 51.5% and 14.9% of participants (N=451; mean age 46 years, 82% Black, 92% female) met the criteria for polypharmacy and hyperpolypharmacy, respectively (Figure 1). Both polypharmacy and hyperpolypharmacy were more common in older participants; polypharmacy was more common in men than women (Figure 1). After adjustment, older age (53.7% and 54.7% vs. 39.9%), male sex (71.5% vs. 49.5%), and higher disease activity (59.4% vs. 44.5%) and cumulative disease damage (62.1% vs. 44.4%) were associated with higher percentages of polypharmacy (Figure 2). Lupus medications (hydroxychloroquine, steroids, and other DMARDs) were common overall (Figure 3) and in those with and without polypharmacy [median number of lupus medications (25th-75th percentiles)=2 (1-3) and 1 (1-2), respectively]. However, cardiovascular medications (especially anti-hypertensives), antacids (including proton pump inhibitors), pain medications, asthma and allergy medications, and anti-depressants all contributed substantially to polypharmacy and hyperpolypharmacy (Figure 3).
Conclusion: Polypharmacy is common in individuals with SLE, particularly among older adults, men, and those with more disease activity and damage. While some medications contributing to polypharmacy are essential treatments for SLE, many are prescribed for common comorbid conditions or pain management. These results suggest that, while multiple medications may be warranted in many cases to treat SLE and its associated comorbidities, there may be opportunities to mitigate polypharmacy overall in this population, by regular reconciliation of medications and exploration of evidence-based non-pharmacologic interventions for symptoms such as pain, acid reflux, and allergy in eligible patients.
To cite this abstract in AMA style:
Yang J, Yazdany J, Lim S, Pearce B, Plantinga L. Prevalence and Potential Factors Associated with Polypharmacy in Individuals with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-potential-factors-associated-with-polypharmacy-in-individuals-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-potential-factors-associated-with-polypharmacy-in-individuals-with-systemic-lupus-erythematosus/