Session Information
Date: Monday, November 9, 2020
Session Type: Abstract Session
Session Time: 12:00PM-12:50PM
Background/Purpose: Peripheral musculoskeletal manifestations in patients with Psoriatic Arthritis (PsA) have been widely studied. However, there is a lack of knowledge on the distribution of such manifestations in the whole group of spondyloarthritis (SpA) and specifically in axial SpA (axSpA), even though an important overlap exists between SpA subtypes and PsA. The ASAS-PerSpA study aimed to evaluate the prevalence, characteristics and treatment of peripheral musculoskeletal manifestations in patients with axSpA and peripheral SpA (pSpA) as well as in PsA across regions of the world.
Methods: Data was collected cross-sectionally in an international multicentre study with 24 participating countries. Consecutive patients diagnosed as having axSpA, pSpA, PsA, inflammatory bowel disease-associated SpA (SpA-IBD), reactive arthritis (ReA), juvenile SpA (JuvSpA) or other form of SpA were eligible for the study. Data concerning the presence of peripheral musculoskeletal manifestations, their localization and specific treatments were collected.
Results: A total of 4465 patients were included (61% men, mean (SD) age of 45 (14) years). Patients came from four geographic areas: Latin America (12.0%), Europe and North America (37.6%), Asia (21.8%) and Middle East and North Africa (28.6%). The most prevalent clinical diagnosis was axSpA (60.9%), followed by PsA (23.1%), pSpA (9.7%), SpA-IBD ( 2.5%), ReA (1.3%), JuvSpA (1.2%) and others (1.3%).
The prevalence of musculoskeletal manifestations were plotted against geographic area and diagnosis in Figures 1 and 2. The most prevalent peripheral manifestation was peripheral articular involvement (excluding root joints) (56.9%) (Figure 1, whole population), with polyarticular involvement more often found in PsA (58.9%) and monoarticular involvement in axSpA (20.1%) (Fig.2). Predominantly upper limb- and small joint involvement were found more often in PsA (52.0%). Predominantly lower limb- and large joint involvement were found more often in ReA and IBD-SpA (55.9%) and in pSpA (51.2%) (Figure 2). Root joint (i.e., hip or shoulder) involvement was found in 33.7% and, of these, 21.8% had both hip and shoulder involvement. Among the total patients with root joint disease, hip involvement alone was found in 57.1%, being most frequent in axSpA (65.0%). Enthesitis in the different groups ranged between 40.9% and 65.9%, with the lowest prevalence found for axSpA; PsA showed the highest mean number of locations of all episodes of enthesitis (4.3 (4.6)). Finally, the prevalence of dactylitis was 15.3%. Dactylitis of the fingers was more prevalent in the group of ReA and IBD-SpA (75.0%), but a higher prevalence of toe-involvement was found in Juv-SpA (66.7%). Only 8.1%, 12.1% and 14.3% of patients had received local injections of corticosteroids for peripheral enthesitis, dactylitis and root joint involvement, respectively.
Conclusion: Although all types of peripheral manifestations are present in the different subtypes of SpA, this study suggests a high inter-region and inter-diagnosis variability of the prevalence of the various peripheral musculoskeletal manifestations in patients with either SpA or PsA.
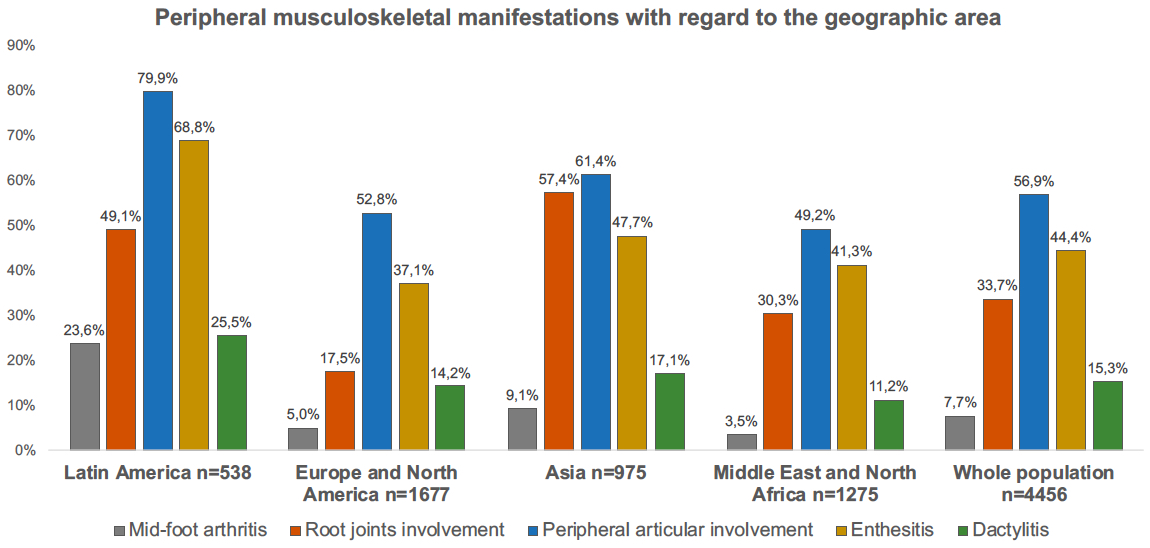 Figure 1. Peripheral musculoskeletal manifestations with regard to the geographic area.
Figure 1. Peripheral musculoskeletal manifestations with regard to the geographic area.
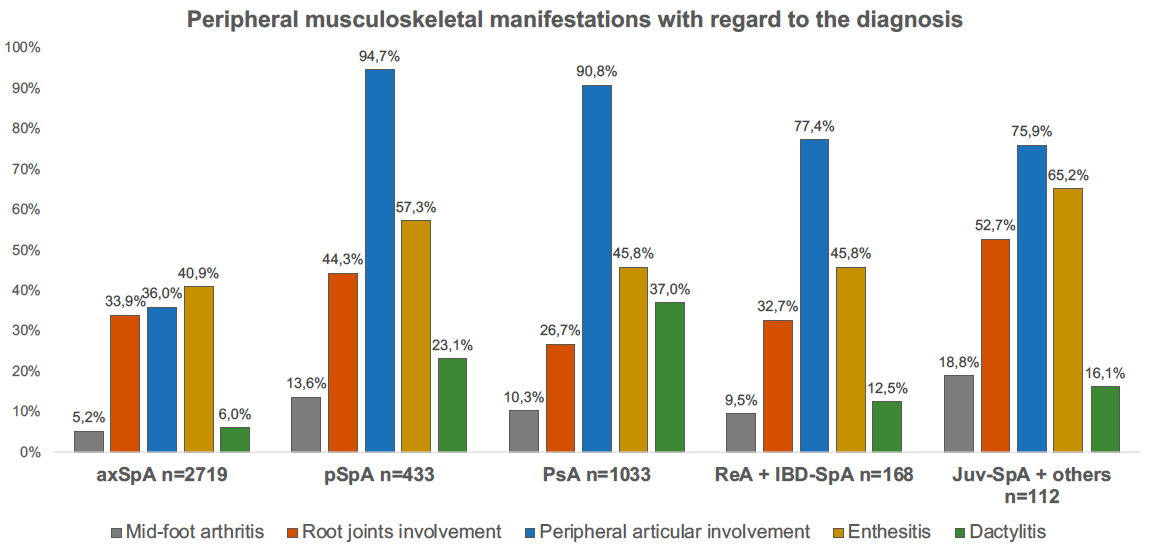 Figure 2. Peripheral musculoskeletal manifestations with regard to the diagnosis.
Figure 2. Peripheral musculoskeletal manifestations with regard to the diagnosis.
To cite this abstract in AMA style:
Lopez-Medina C, Molto A, Sieper J, Duruöz M, Kiltz U, El-Zorkany B, Hajjaj-Hassouni N, Burgos-Vargas R, Maldonado-Cocco J, Ziade N, Gavali M, Navarro-Compán V, Luo S, Monti S, Kim T, Kishimoto M, Pimentel-Santos F, Gu J, Schiotis R, van Gaalen F, Géher P, Magrey M, Ibanez S, Bautista-Molano W, Maksymowych W, Machado P, Landewé R, van der Heijde D, Dougados M. Prevalence and Distribution of Peripheral Musculoskeletal Manifestations in Axial Spondyloarthritis, Peripheral Spondyloarthritis and Psoriatic Arthritis: Results of the International, Cross-sectional ASAS-PerSpA Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-and-distribution-of-peripheral-musculoskeletal-manifestations-in-axial-spondyloarthritis-peripheral-spondyloarthritis-and-psoriatic-arthritis-results-of-the-international-cross-sectional/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-distribution-of-peripheral-musculoskeletal-manifestations-in-axial-spondyloarthritis-peripheral-spondyloarthritis-and-psoriatic-arthritis-results-of-the-international-cross-sectional/
