Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Numerous investigators have demonstrated that the risks of pre-eclampsia, preterm delivery, and fetal death are increased in lupus pregnancies. Adverse events during pregnancy, delivery, and the post-natal period occur for many reasons, and it is often unclear whether they are SLE-related. Furthermore, it is well established that before the clinical diagnosis of SLE, pathogenic autoantibodies are present in individuals who eventually develop lupus, and they may drive inflammation.
Given the challenges in identifying and accessing a proper comparator group, most published work has focused on clinical cohorts and case series. A few studies that used national or population-based data to answer such questions face different methodological limitations – particularly SLE misclassification due to use of a single ICD code to define cases. This work compares pregnancies and outcomes in women with SLE using a stricter classification and considers outcomes in women whose SLE is believed to onset after pregnancy.
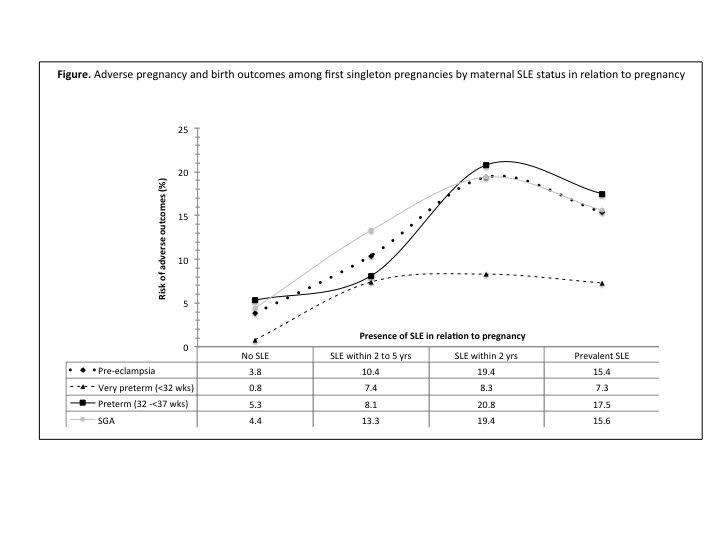
Methods: Data from a matched cohort of individuals with SLE and the general population using national Swedish registers were linked to the Medical Birth Register (MBR) to identify all pregnancies between 1973 and 2011. SLE was defined as ³2 SLE ICD codes in the Patient Register (PR) with ³1 SLE code from a specialist. We restricted to first pregnancy and excluded multiple gestations. Using the first observed SLE interaction with the health care system as a proxy for diagnosis, we categorized SLE as prevalent at birth (n=604), incident within 0-2 (n=72) and 2-5 years (n=135) after birth, and none (n=18229). Maternal health and delivery characteristics were obtained from the MBR, PR, and Death Register. Outcomes included pregnancy morbidity such as pre-eclampsia, maternal death, size for gestational age, APGAR scores, and stillbirth. We compared frequency of outcomes by SLE exposure at pregnancy/birth (prevalent, in 0-2y, in 2-5y, and none). Modified Poisson regression with robust error variance estimated risk ratios and 95% CI with SLE as exposure for maternal and fetal outcomes adjusted for maternal age and other a priori determined confounders.
Results: Patients with SLE were more likely to have poorer pregnancy outcomes including small for gestational age (SGA), preterm deliveries, pre-eclampsia, stillbirths, and lower one minute APGAR compared to the general population. For many outcomes we saw a trend where the closer to pregnancy the diagnosis of SLE was made (with prevalent SLE being most proximal) the higher the risk of poor outcomes (Figure).
Conclusion: Maternal SLE is associated with adverse outcomes to mothers and their newborn. Mothers whose SLE presented shortly after pregnancy also had higher risk of these outcomes compared to pregnancies and births from the general population.
Disclosure:
E. V. Arkema,
None;
K. Palmsten,
None;
C. Sjöwall,
None;
E. Svenungsson,
None;
J. E. Salmon,
None;
J. F. Simard,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pregnancy-outcomes-in-sle-before-and-after/