Session Information
Date: Sunday, November 8, 2020
Session Type: Plenary Session
Session Time: 11:30AM-1:00PM
Background/Purpose: Patients with interstitial lung disease (ILD) are often recommended to avoid conception or terminate pregnancy despite limited data on pregnancy outcomes and complications. Studies to date have only been conducted in small samples of 9-15 patients with mixed results. This study aims to retrospectively analyze pregnancy outcomes in the largest-to-date cohort of patients with ILD secondary to autoimmune disease to further inform providers and patients on the risks of pregnancy. We hypothesize that patients with more severe ILD as classified by physiologic measures will have worse pregnancy outcomes and increased complications.
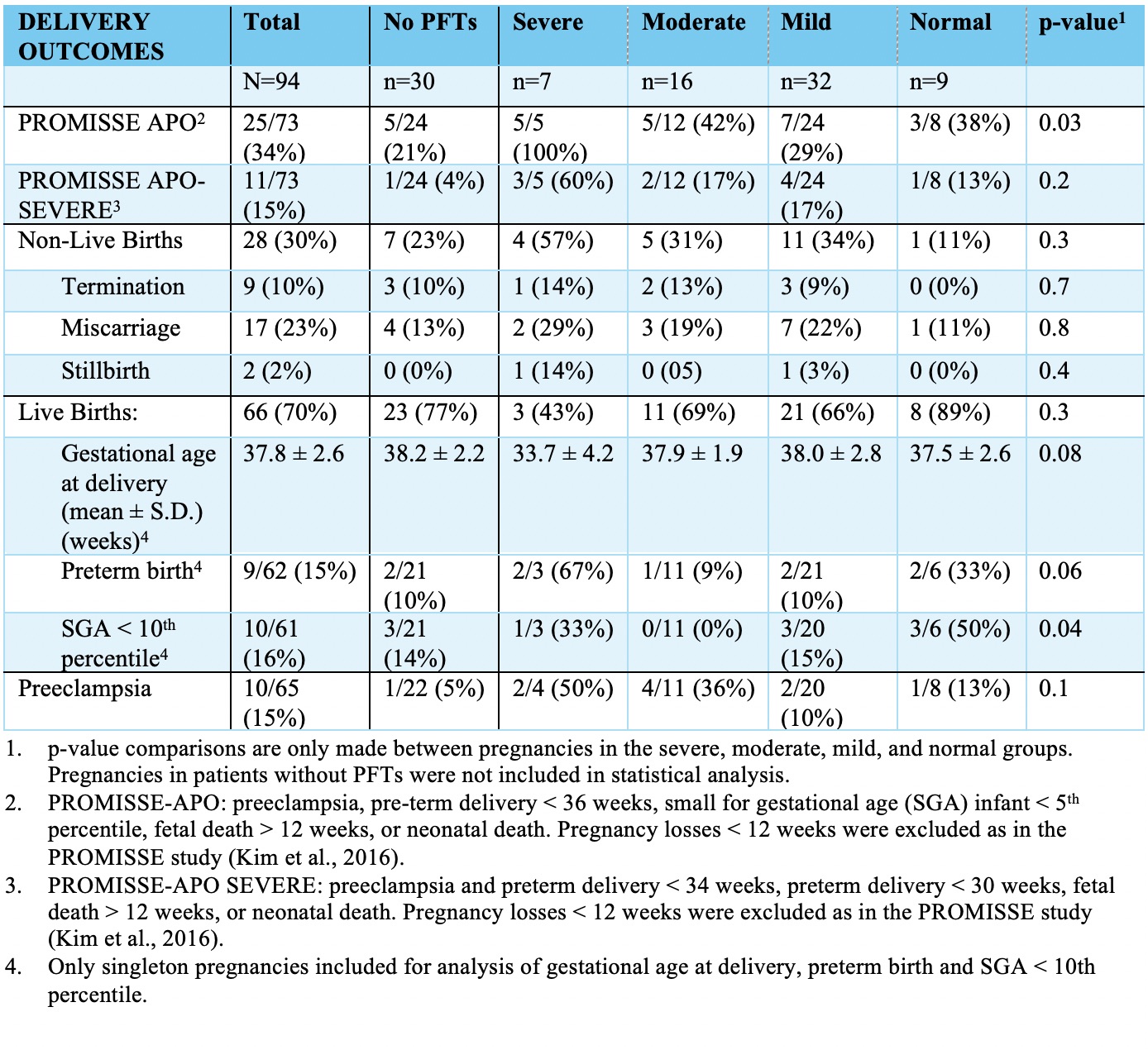
Methods: Medical records in the Duke University Health System (1/1/1996 – 7/1/2019) were reviewed for pregnancies in patients with a diagnosis of ILD secondary to autoimmune disease. Pregnancies were classified according to severity of ILD based on percent predicted forced vital capacity (FVC % pred) or percent predicted diffusion capacity for carbon monoxide (DLCO % pred). Cutoff values included normal (DLCO % pred ≥ 80% and FVC % pred ≥ 80%), mild (DLCO % pred 61-79% or FVC % pred 60-79%), moderate (DLCO % pred 40-60% or FVC % pred 40-59%), and severe (DLCO % pred < 40% or FVC % pred < 40%). Adverse outcomes were defined using the composite PROMISSE-APO (preeclampsia, pre-term delivery < 36 weeks, small for gestational age (SGA) infant < 5th percentile, fetal death > 12 weeks, or neonatal death) and PROMISSE-APO SEVERE (preeclampsia and preterm delivery < 34 weeks, preterm delivery < 30 weeks, fetal death > 12 weeks, or neonatal death). Fisher’s Exact Test and ANOVA was used to compare outcomes among patients in different severity groups.
Results: This study included 67 patients with 94 pregnancies (5 twin pergnancies). The average maternal age was 32.1 ± 6.0 years with 83% identifying as Black. Overall, 69% of pregnancies were diagnosed with sarcoidosis and the remaining 31% had a connective tissue disease associated ILD (CTD-ILD). Of the pregnancies with available measures to classify ILD severity (n=64), 11% were severe, 25% were moderate, 50% were mild, and 14% were normal. All the pregnancies in the severe group had CTD-ILD while 89% of pregnancies in the normal group had sarcoidosis (p=0.001 across groups).
Overall, 70% of pregnancies resulted in live births and 9 pregnancies (10%) were terminated (Fig. 1). There was a 15% rate of pre-eclampsia, 34% rate of PROMISSE-APO, and 15% rate of PROMISSE-APO SEVERE. Patients with severe disease had the highest rates of PROMISSE-APO (p=0.03 across groups).
There were no maternal deaths and only 2 pregnancies required intensive care unit care. Overall, 4 pregnancies experienced volume overload at the time of delivery, of which 1 patient developed postpartum heart failure. A total of 8 pregnancies required oxygen at the time of delivery, and 1 patient was intubated during pregnancy.
Conclusion: While adverse pregnancy outcomes are common in ILD pregnancies, especially in patients with more severe disease, overall maternal morbidity and mortality is low. Patients with ILD do not necessarily have to terminate pregnancies provided they have close monitoring before, during, and after pregnancy and appropriate subspecialist involvement.
To cite this abstract in AMA style:
Rajendran A, Giattino S, Eudy A, Swaminathan A, Clowse M. Pregnancy Outcomes in Patients with Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/pregnancy-outcomes-in-patients-with-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pregnancy-outcomes-in-patients-with-interstitial-lung-disease/