Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Women with systemic lupus erythematosus (SLE) have increased rates of pre-term birth, small for gestational age babies, and pre-eclampsia compared to women without a diagnosis of SLE. Ongoing research has shown a dysregulated immune system, adversely affects patients even if SLE is not yet diagnosed suggesting a “pre-SLE disease state” exists. We hypothesize that a pre-SLE disease state impacts pregnancy outcomes among women with circulating SLE-associated autoantibodies prior to a diagnosis of SLE.
Methods: Case control study including women with at least one prior recorded pregnancy from an ongoing longitudinal SLE registry at a single center. Controls (related/family member or unrelated) were included if unaffected by SLE. The registry has been enrolling since 2003 with baseline and follow up visits. Information on demographics, pregnancy history, social, family, and medical histories was obtained through in person interviews and chart review. Comorbidities were counted if present at any time in the registry. All SLE patients included met ACR classification criteria for the disease. Associations between different pregnancy outcomes with patient-pregnancy type and demographic variables were evaluated with univariate and multivariable modeling.
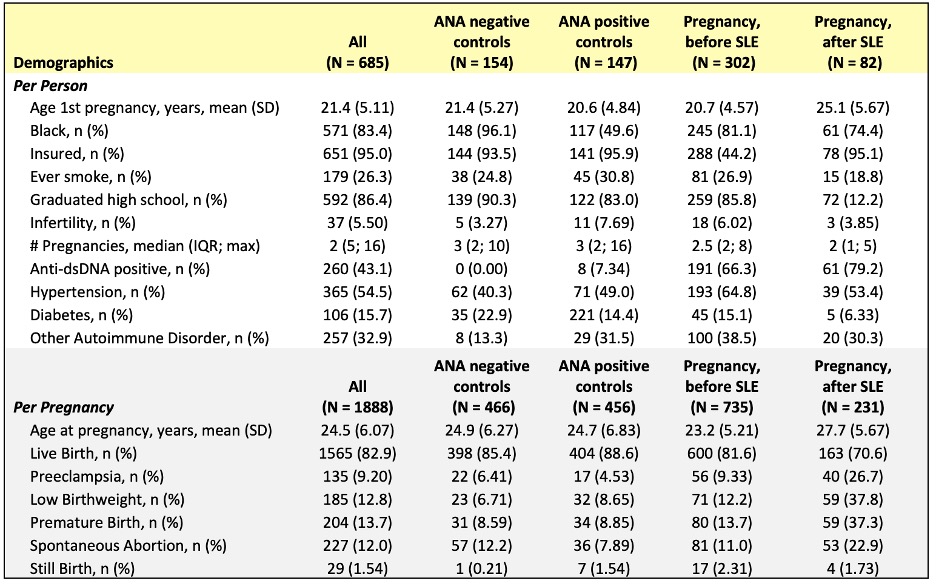
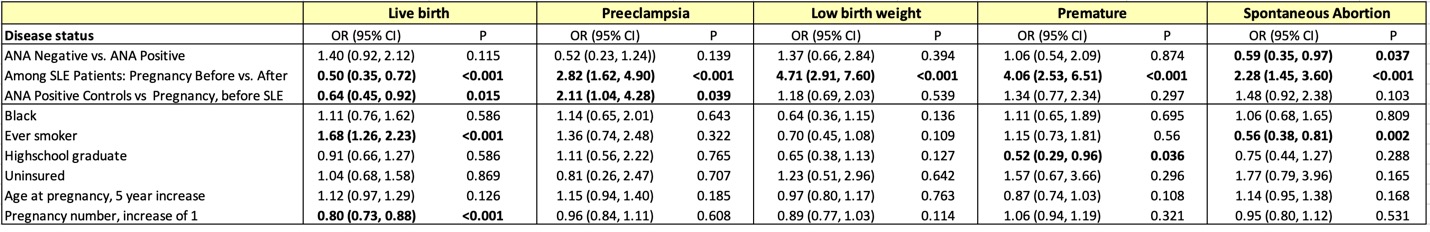
Results: 685 women (SLE and controls) were included in our analysis with 1888 pregnancies, Table 1. Of those, 302 women (735 pregnancies) were prior to a diagnosis of SLE. A higher proportion of related controls were ANA positive (47.7%) as compared to unrelated controls (30.5%). Overall, 83% of women self-identified at Black. Multivariable analysis revealed no differences in ANA positive versus negative controls in odds of live birth, preeclampsia, low-birthweight, premature delivery, Table 2. Those with pregnancies prior to a diagnosis of SLE had lower odds of live birth, OR 0.64 (0.45-0.92) and increased odds of preeclampsia, OR 2.11 (1.04-4.28) as compared to ANA positive controls. There were no significant differences in this group for outcomes of low birth weight, premature birth, or spontaneous abortion. Pregnancy outcomes were worse in all categories for women who had pregnancies after a diagnosis of SLE, the highest being low birth weight, OR 4.71 (2.91-7.60), and premature birth, OR 4.06 (2.53, 6.51).
Conclusion: In a large SLE cohort, we note differences in pregnancy outcomes among women with SLE compared to two groups of controls. Women prior to their diagnosis of SLE had fewer live births (81.6 vs 88.6%) and higher preeclampsia risk (9.3% vs 4.5%) compared to ANA positive controls, which remained statistically significant after controlling for race, smoking, education, insurance, age and multiparity. A pre-disease state, beyond ANA positivity, may exist increasing pregnancy risk before the diagnosis of SLE in some patients. Analysis incorporating timing of additional autoantibody development and comorbidities is ongoing. These results support continued investigations of additional immunologic and epidemiologic factors which may ultimately affect pregnancy outcomes in women who are diagnosed with SLE.
To cite this abstract in AMA style:
English J, Wolf B, Kamen D. Pregnancy Outcome Disparities Among Women with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pregnancy-outcome-disparities-among-women-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pregnancy-outcome-disparities-among-women-with-systemic-lupus-erythematosus/