Session Information
Date: Monday, November 9, 2020
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Giant cell arteritis (GCA) is the most common primary vasculitis in patients (pts) aged over 50 years. It is a medical emergency due to the potential occurrence of severe ischaemic events (SIEs), namely vision loss (VL) and cerebrovascular accidents (CVAs), largely responsible for the high burden of this disease. Identifying patients at a higher risk of developing VL and CVAs is clinically relevant to determine prognosis and tailor treatment.
Methods: Bicentric observational retrospective study using data from the Rheumatic Diseases Portuguese Registry (Reuma.pt). Pts with biopsy or ultrasound-proven GCA were included. VL and CVAs (stroke or transient ischaemic attacks) were considered the SIEs of interest. Clinical features of patients with or without SIEs were compared using Chi-square and Mann-Whitney U tests, as appropriate; multivariate logistic regression was used to identify predictors of SIEs.
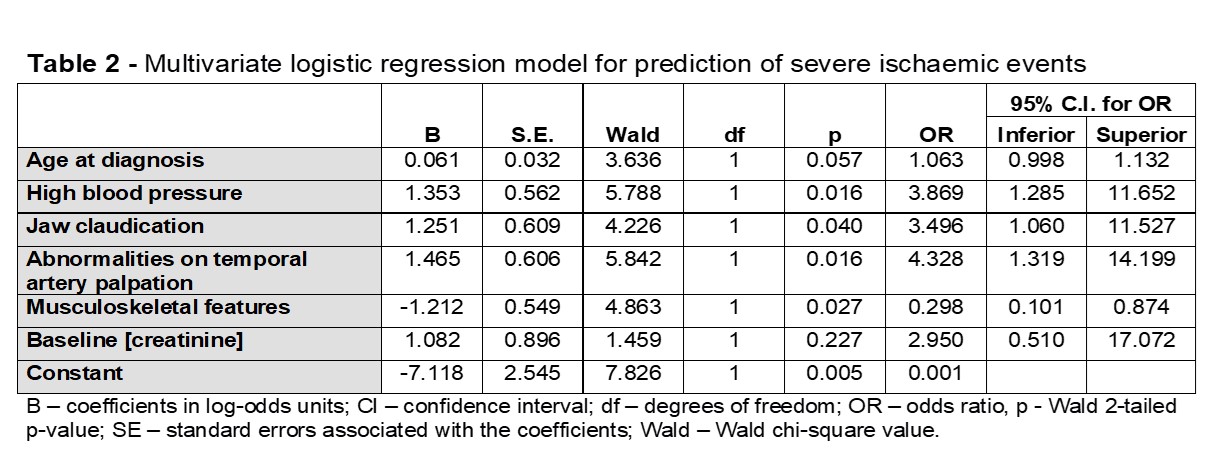
Results: A total of 134 pts diagnosed with GCA between 1998 and 2019 were included. Median (IQR) age at diagnosis was 76.4 (70.2-82.4) years and 66% of pts were females. At least one SIE was reported in 65 (48.5%) pts; 8 pts had more than one SIE. A total of 73 SIEs were recorded: 44 cases of ischaemic optic neuropathy (29 anterior, 2 posterior, 13 not specified), 61% with unilateral involvement and 74% leading to permanent visual loss (PVL); 6 cases of central retinal artery occlusion with 100% PVL; 16 ocular events of non-specified cause (6 transient visual loss, 5 PVL, 5 diplopia); 6 ischeamic strokes; and 1 transient ischaemic attack. Table 1 presents the differences between pts with and without SIEs. On univariate analyses, pts with SIEs were older (p< 0.001), and more often had previous hypertension (OR: 3.0, 95%CI: 1.4-6.3), jaw claudication (OR 3.0, 95%CI: 1.5-6.5) and temporal artery (TA) abnormalities on clinical examination (OR 4.5, 95%CI: 1.8-10). By contrast, musculoskeletal (MSK) features including polymyalgia rheumatica (PMR) were negatively associated with the occurrence of SIEs (OR 0.37, 95%CI: 0.2-0.7). In terms of laboratory results, only creatinine levels at diagnosis were significantly higher (p=0.014) in pts with SIEs; no differences were seen between groups for baseline inflammatory markers or haemoglobin levels. Likewise, antiplatelet therapy started before GCA diagnosis did not seem to prevent severe SIEs. By multivariate logistic regression (Table 2), hypertension, jaw claudication and abnormalities of TA on palpation were independently associated with SIEs. The presence of MSK symptoms significantly decreased the risk of SIEs.
Conclusion: Almost half the pts in this cohort presented VL and/or CVAs, highlighting the need for an earlier recognition of symptoms and a fast-track approach to pts with suspected GCA to improve outcome. High blood pressure, jaw claudication and abnormalities of TA on palpation were associated with an increased risk of SIEs, while the presence of MSK symptoms including PMR had a protective role. The identification of pts with these high-risk features should prompt immediate treatment and tight follow-up. Future studies are warranted to determine the value of more aggressive immunosuppression in these cases.
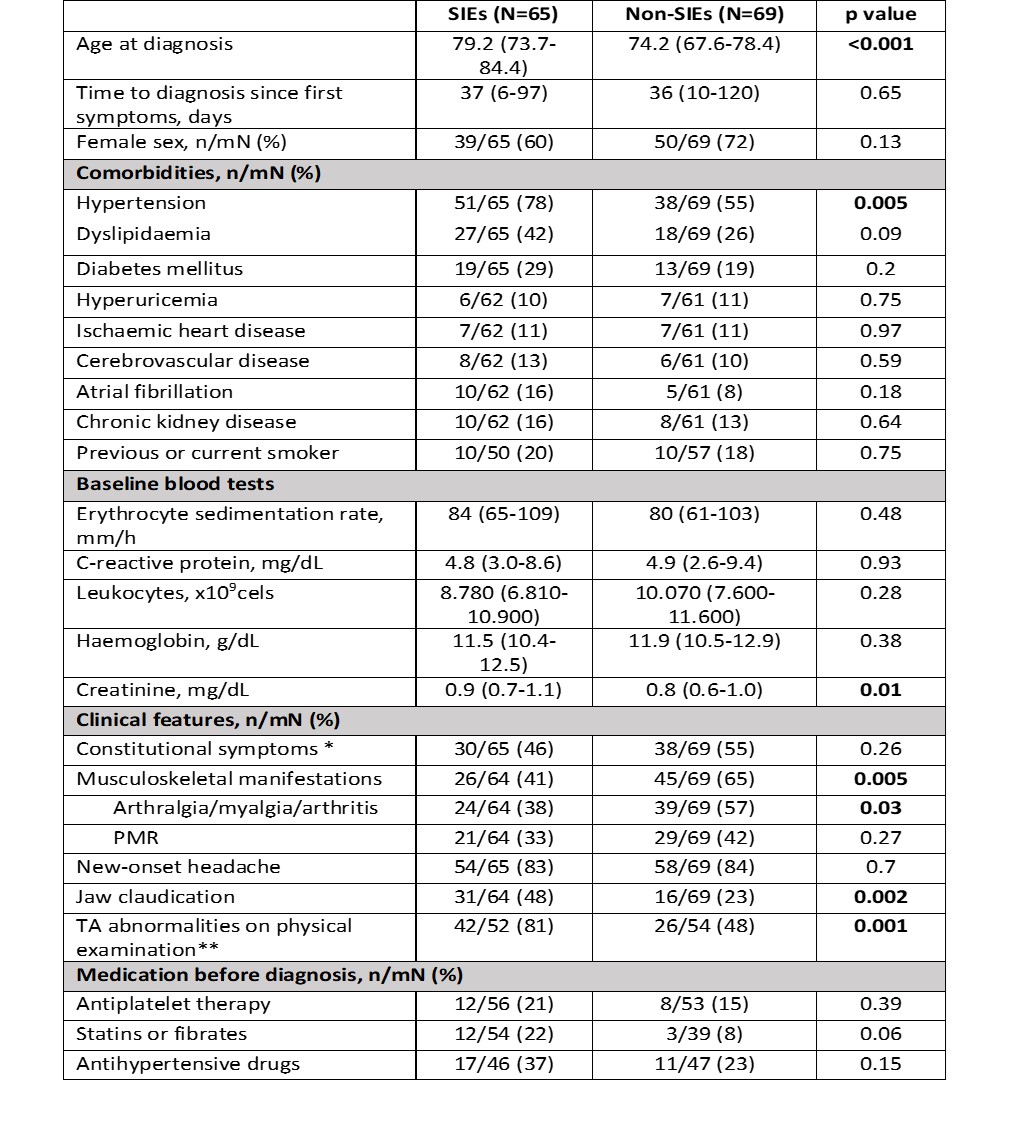 Table 1: Differences between GCA patients with and without severe ischaemic events. SIEs: severe ischaemic events; GCA: Giant cell arteritis; PMR: polymyalgia rheumatica; TA: temporal artery. Continuous variables are expressed as median (IQR). Categorical variables are expressed as n/modified(m)N (total N -missing data), %. * Fatigue, anorexia, weight-loss, fever, night sweats or lymphadenopathies. ** Thickness, tenderness, and reduced or absent pulse.
Table 1: Differences between GCA patients with and without severe ischaemic events. SIEs: severe ischaemic events; GCA: Giant cell arteritis; PMR: polymyalgia rheumatica; TA: temporal artery. Continuous variables are expressed as median (IQR). Categorical variables are expressed as n/modified(m)N (total N -missing data), %. * Fatigue, anorexia, weight-loss, fever, night sweats or lymphadenopathies. ** Thickness, tenderness, and reduced or absent pulse.
To cite this abstract in AMA style:
Cruz-Machado A, Barreira S, Dourado E, Martinho J, Raimundo D, Brites L, Assunção H, Teixeira V, Khmelinskii N, Macieira C, da Silva J, Fonseca J, Ponte C. Predictors of Visual Loss and Cerebrovascular Accidents in Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/predictors-of-visual-loss-and-cerebrovascular-accidents-in-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-visual-loss-and-cerebrovascular-accidents-in-giant-cell-arteritis/