Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Renal involvement in the context of anti-neutrophil cytoplasm antibody (ANCA)-associated vasculitis (AAV) is associated with significant morbidity and higher mortality rates. This study examined predictive factors associated of renal involvement in AAV within a large, international cross-sectional cohort.
Methods: Univariate and multivariate analyses were performed to identify risk factors associated with renal disease, which was defined as i) an increase of serum-creatinine > 30%; ii) a fall in creatinine-clearance < 25%; or iii) haematuria attributable to active vasculitis.
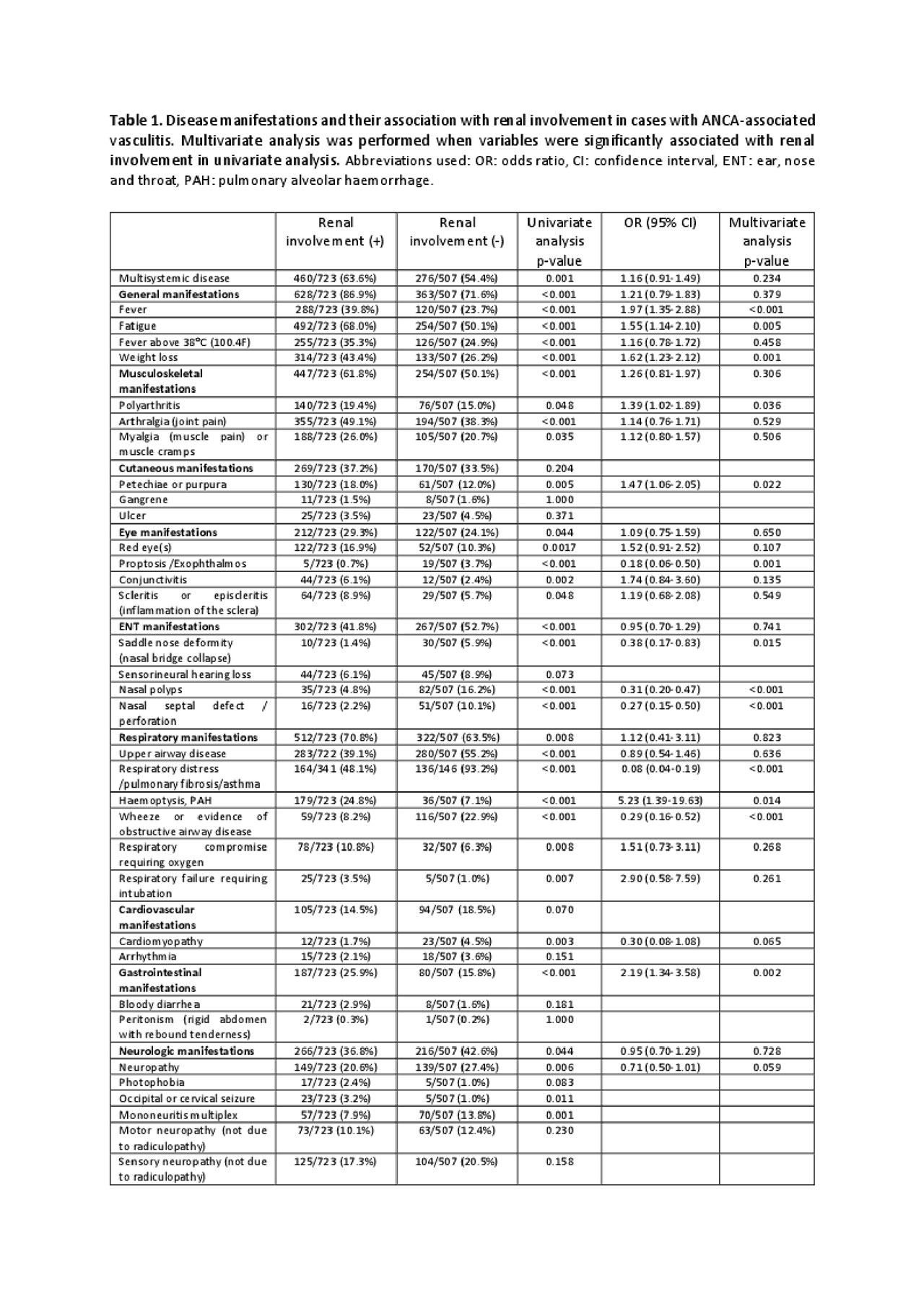
Results: Of the 1230 patients eligible, 723 patients (58.8%) presented with renal involvement. The majority of patients with microscopic polyangiitis (82.2%) and granulomatosis with polyangiitis (58.6%) had renal involvement, while 26.4% with eosinophilic granulomatosis with polyangiitis presented with renalvasculitis. The following clinical factors were more common among patients with renal disease that among patients without renal disease. Older age (57.9 versus 53.9 years, p=0.001), fever (39.8% versus 23.7%, p< 0.001), fatigue (68.0% versus 50.1%, p=0.005), weight loss (43.4% versus 26.2%, p=0.001), polyarthritis (19.4% versus 15.0%, p=0.036), petechiae/purpura (18.0% versus 12.0%, p=0.022), pulmonary haemorrhage (24.8% versus 7.1%, p=0.014), gastrointestinal symptoms (25.9% versus 15.8%, p=0.002), serum albumin below 30 g/L (36.6% versus 11.6%, p< 0.001), higher CRP (105.86 ± 96.56 versus 54.25 ± 61.60, p=0.038), low C3 at baseline (7.6% versus 2.9%, p=0.015), ANCA positivity (p< 0.001), myeloperoxidase-ANCA (43.9% versus 29.6%, p< 0.001) and proteinase 3-ANCA (48.4% versus 40.5%, p=0.020).Patients with proptosis/exophthalmos (0.7% versus 3.7%, p=0.001), saddle nose deformity (1.4% versus 5.9%, p=0.015), nasal polyps (4.8% versus 16.2%) and nasal septal defect/perforation (2.2% versus 10.1%) (p< 0.001 each), respiratory distress/pulmonary fibrosis/asthma (48.1% versus 93.2%, p< 0.001) or wheeze/obstructive airway disease (8.2% versus 22.9%, p< 0.001) had a lower likelihood of developing renal involvement. (see Table 1 and Table 2).
Conclusion: In this large international study, we identified clinical factors associated with renal involvement in AAV, including concomitant pulmonary alveolar haemorrhage, low C3, and elevated C-reactive protein. Further large studies arenecessary to confirm our findings.
To cite this abstract in AMA style:
Kronbichler A, Shin J, Lee K, Nakagomi D, Quintana L, Busch M, Craven A, Luqmani R, Merkel P, Mayer G, Jayne D, Watts R. Predictors of Renal Involvement in ANCA-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/predictors-of-renal-involvement-in-anca-associated-vasculitis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-renal-involvement-in-anca-associated-vasculitis/