Session Information
Date: Sunday, November 7, 2021
Title: Pediatric Rheumatology – Clinical Poster II: SLE, JDM, & Juvenile Scleroderma (0764–0785)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Childhood-onset Systemic lupus erythematosus (cSLE) is an inflammatory autoimmune disease known for its complex and variable clinical presentation and disease course. Its severity may vary according to different organs involved and is usually life-threatening and have poorer outcome compared to adults (aSLE), leading to significant morbidity and mortality. The objectives of this study were to identify predictors of mortality of cSLE and to evaluate their association with clinical manifestations, laboratory features, disease activity and damage, current treatment, survival and causes of death.
Methods: This is a multicenter, nationwide observational study of a cohort of 1,528 cSLE patients followed in 27 Brazilian pediatric rheumatology tertiary centers. In this study, we investigated cumulative risk factors for mortality in a large sample of cSLE patients. We also compared its association with cumulative clinical and laboratory features, as well as disease activity and damage, cumulative treatment, outcome and causes of death.
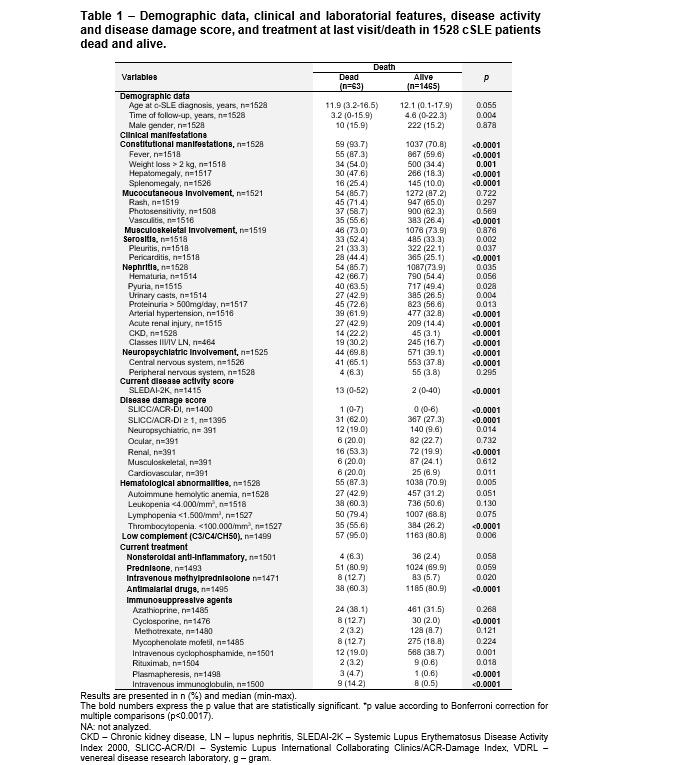
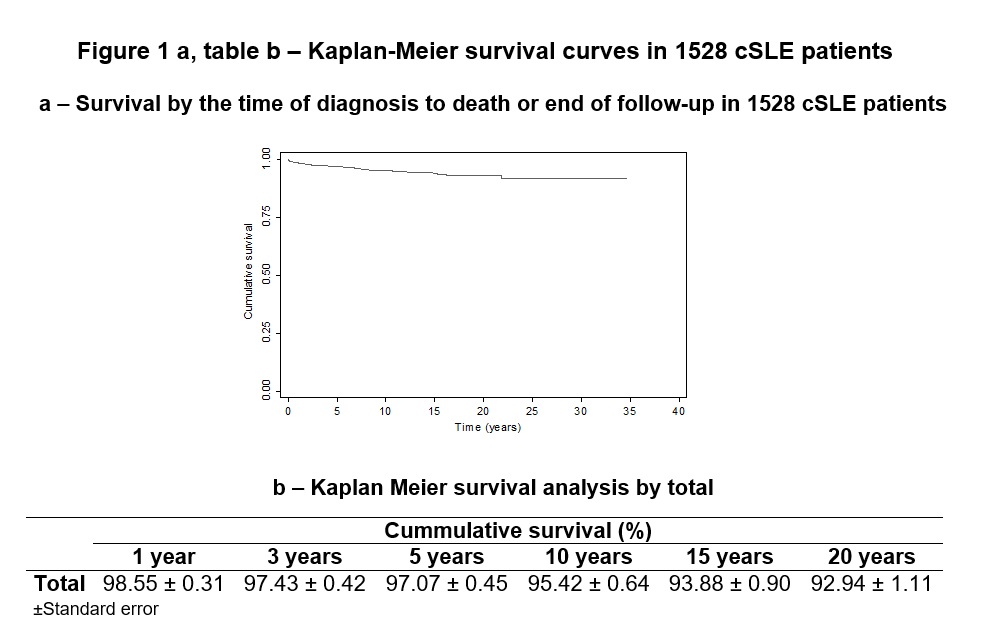
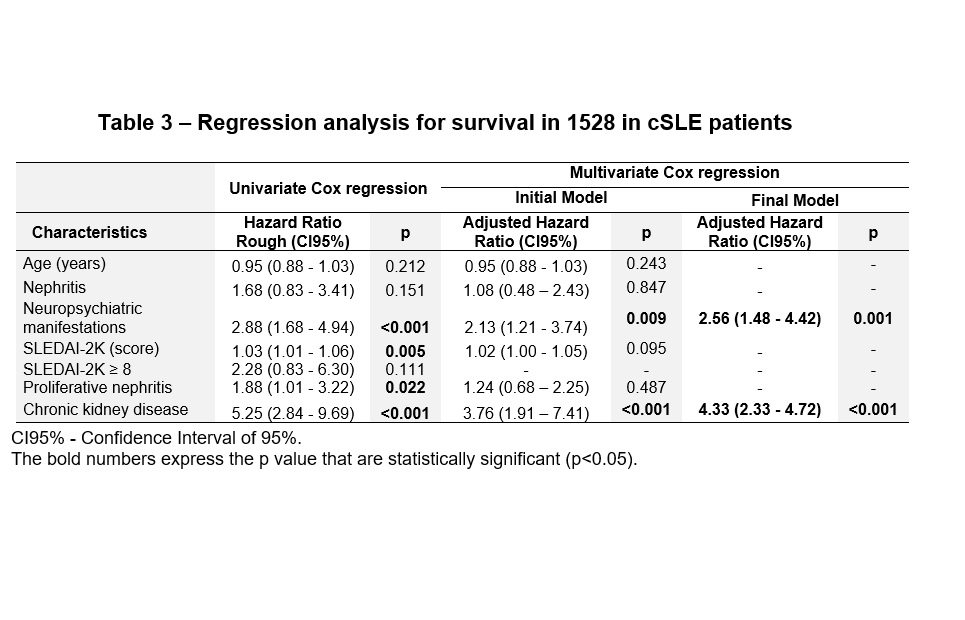
Results: Mortality between patients was 4.1% (63/1528), occurring in a median period of 3.2 years after diagnosis, with predominance of girls (84.1%). The most frequent causes of death were sepsis/infectious disease in 29/63 (29%) and cSLE activity in 8/63 (12.7%). In 12/63 (19%) the cause was unknown. After Bonferroni´s correction for multiple comparisons (p˂0.0017), determinants significantly associated with mortality were constitutional symptoms, skin vasculitis, pericarditis, arterial hypertension, acute renal injury, chronic kidney disease (CKD), neuropsychiatric (NP-SLE), thrombocytopenia, higher score of SLEDAI-2K at last visit or death, and SLICC/ACR-DI especially in renal domain. The use of intravenous methylprednisolone, cyclosporine, cyclophosphamide, and rituximab at last visit or death were also more frequent. In the multivariate regression model analysis, NP-SLE (p=0.001) and CKD (p= ˂0.0001) were significant factors associated to death. Patients with NP-SLE had 2.6 times higher risk of death (HR=2.56, 95%CI=1.48-4.42) compared to cSLE patients who did not present NP-SLE, and the risk of death in patients with CKD increases 4.3 times (HR=4.33, 95%CI=2.33-8.04). The Kaplan-Meier overall curve showed worse survival in patients with NP-SLE (p=˂0.0001), proliferative nephritis (p=0.02) and CKD (p=˂0.0001). Overall patient survival after diagnosis at 1, 5 and 10 years were 98.5%, 97% and 95.4% respectively.
Conclusion: This study showed that cSLE patients with CKD and NP-SLE exhibited higher hazard rates of progression to poor outcomes. Therefore, those patients could benefit from early aggressive management of active lupus nephritis and NP-SLE, especially within the first years after diagnosis.
To cite this abstract in AMA style:
Sakamoto A, Silva C, Islabão A, Novak G, Molinari B, Pereira R, Saad-Magalhães C, Clemente G, Fraga M, Pioto D, Len C, do Prado R, Terreri M. Predictors of Mortality in a Series of 1528 Brazilian Childhood-onset Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/predictors-of-mortality-in-a-series-of-1528-brazilian-childhood-onset-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-mortality-in-a-series-of-1528-brazilian-childhood-onset-systemic-lupus-erythematosus-patients/