Session Information
Date: Monday, November 8, 2021
Title: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster (1135–1149)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: A virtual bone health team (BHT) model was implemented to identify, screen, and treat rural Veterans at risk for osteoporosis. This study was conducted to identify social determinants of health and clinical factors associated with osteoporosis screening through enrollment in the BHT clinic and with osteoporosis medication initiation among those with a treatment indication.
Methods: Eligibility for BHT included: ages 50 to 99; enrollment in VA primary care; and either medication, age, or osteoporosis self-assessment tool score- based risk. A cross-sectional cohort design was utilized with a generalized estimating equation (GEE) and logit link function to account for facility-level clustering. Fully saturated and reduced models were fit using backward selection. Given population size and high percentage of medication initiators, contingency tables were constructed, and the Fisher’s exact test was performed to understand medication initiation.
Results: The cohort comprised 6985 rural Veterans. Twenty-two percent accepted dual-energy X-ray absorptiometry (DXA) and were male (94%), white (95%), and married (69%), with a mean age of 76 (Table 1). Multivariate models suggest that age, distance from VA services, race, marital status, co-payment, prior fracture, or history of rheumatoid arthritis are significantly associated with DXA acceptance (Table 2). Of those with indication for medication (N=453), most were male and white, with mean age of 77 (Table 3). Few had prior DXA or osteoporosis medication, one-third had prior corticosteroid use. Fisher’s exact test results suggest that a history of 2 or more falls in the prior year, current smoking, weight-bearing exercise, and parental history of hip fracture are all associated with osteoporosis medication initiation.
Conclusion: The BHT model facilitated DXA for rural Veterans at their nearest VA or non-VA facility, but cost and travel remain barriers to DXA in addition to other social determinants of health such marital status, race, and gender. Some known osteoporosis risk factors were associated with lower acceptance of DXA. Age, distance, marital status, and race were not associated with medication initiation, while the proportion of rural Veterans with a history of falls or smoking was greater for those who initiated medication. Further efforts are needed to gain insight into how clinical and social factors impact perception of risk and how health care systems can incorporate social determinant of health and clinical predictors of bone health care engagement to improve bone health care delivery across a variety of contexts.
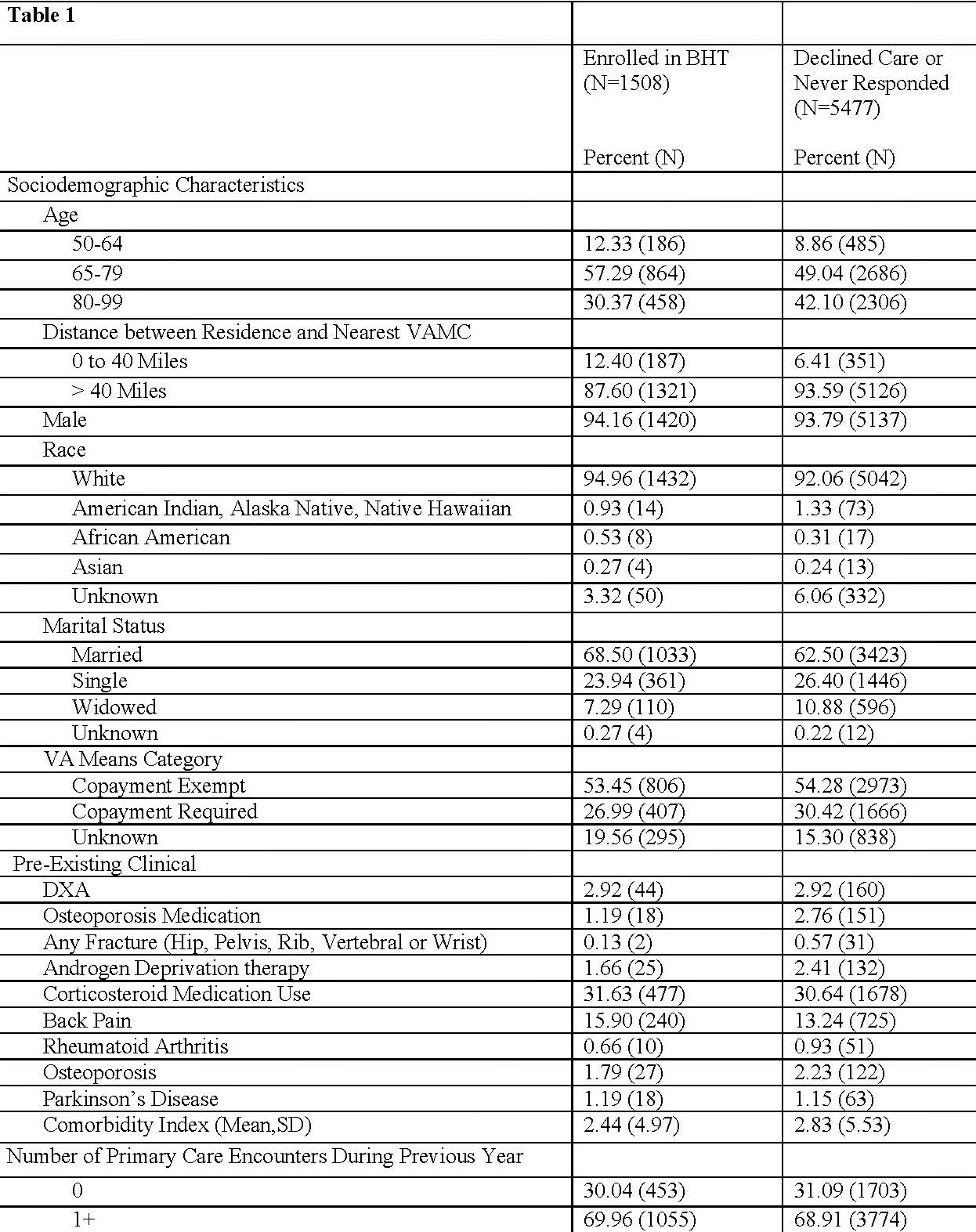 Sociodemographic and Clinical Characteristics of Eligible Veterans by Decision to Enroll
Sociodemographic and Clinical Characteristics of Eligible Veterans by Decision to Enroll
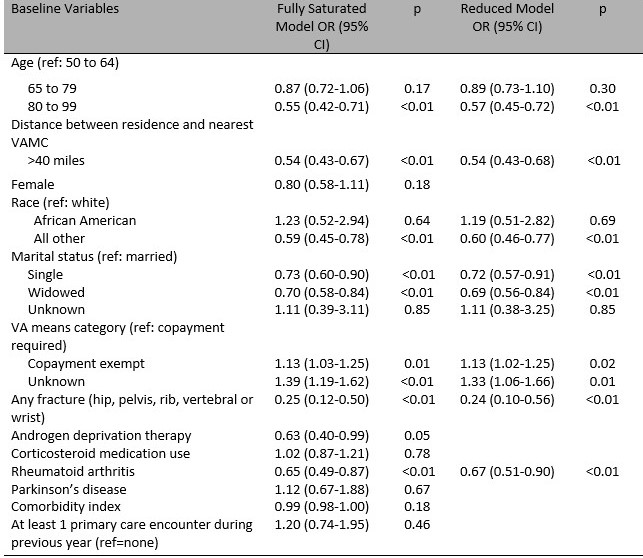 Multivariate Logistic Regression Model Predicting BHT Enrollment
Multivariate Logistic Regression Model Predicting BHT Enrollment
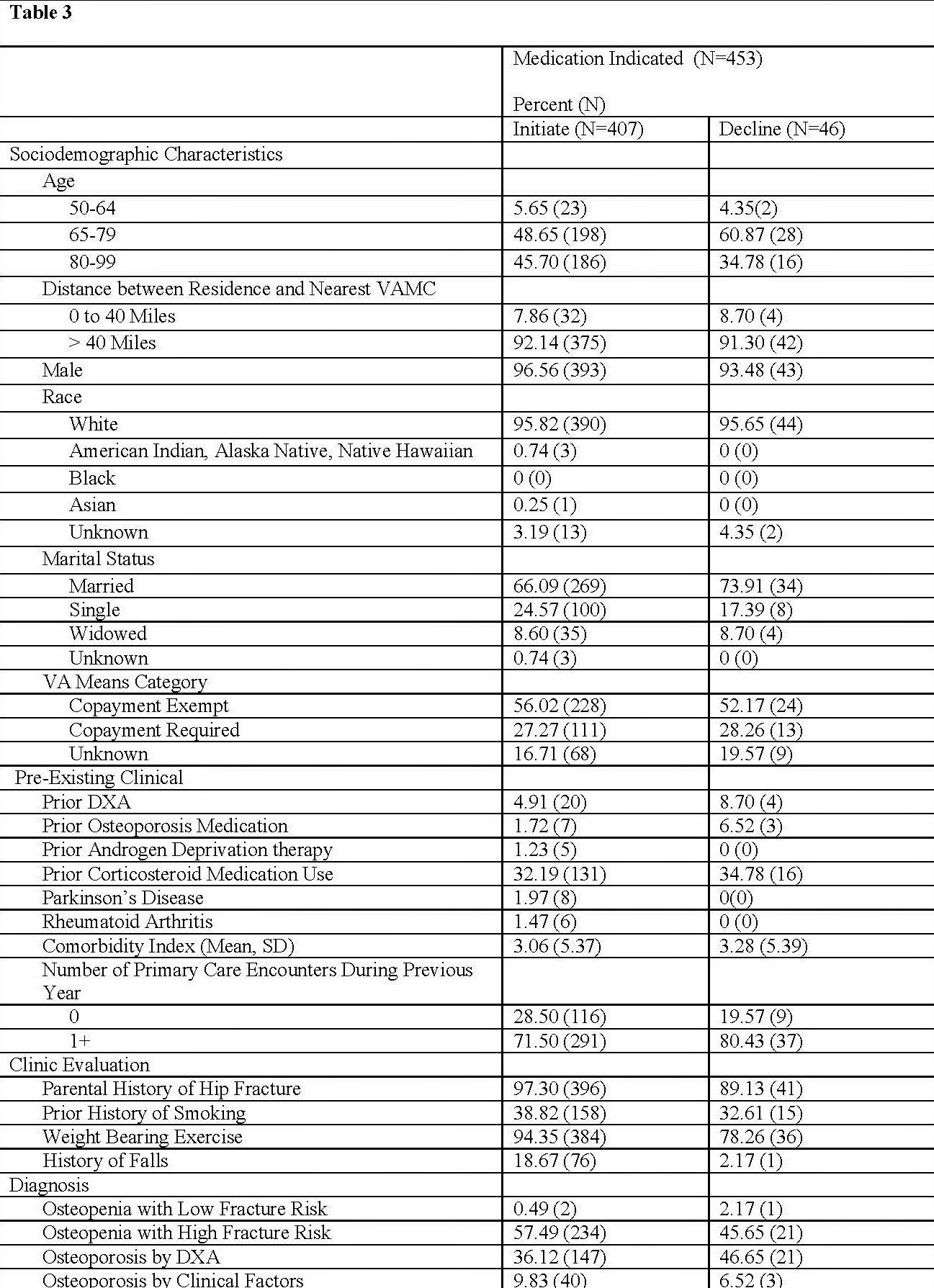 Veteran Characteristics by Response to Treatment Recommendations for Those Enrolled in BHT
Veteran Characteristics by Response to Treatment Recommendations for Those Enrolled in BHT
To cite this abstract in AMA style:
Miller K, McCoy K, Richards C, Seaman A, Solimeo S. Predictors of Engagement in Bone Health Care Among Rural Veterans at Risk for Osteoporosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/predictors-of-engagement-in-bone-health-care-among-rural-veterans-at-risk-for-osteoporosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-engagement-in-bone-health-care-among-rural-veterans-at-risk-for-osteoporosis/
