Background/Purpose: Experts recommend discussing modifiable cardiovascular disease (CVD) risk factors in RA visits. We examined the predictors of discussions about cholesterol and or lifestyle (weight, diet, exercise) in RA visits among patients eligible for improved cholesterol control, and compared them to other prevention topics: vaccination, bone health. We hypothesized that cholesterol/lifestyle discussions would depend on perceived RA control at a given visit.
Methods: Electronic health records were used to identify RA patients with uncontrolled cholesterol who received primary and rheumatology care in a health system with 3 rheumatology clinics (2004-2011). Those with diabetes, CVD, chronic kidney disease with low density lipoprotein (LDL) cholesterol >100 mg/dL and without such conditions whose LDL exceeded 130 mg/dL had visit notes reviewed by trained abstractors until LDL control or censoring for loss of continuity, death, or end of data. “RA control” was defined as stated by a rheumatologist in the visit note. We used logistic regression to calculate the odds ratios (OR) and 95% confidence intervals reflecting RA control as a predictor of cholesterol/lifestyle or other prevention discussions after controlling for sociodemographics, comorbidity (ACG score), and clinic.
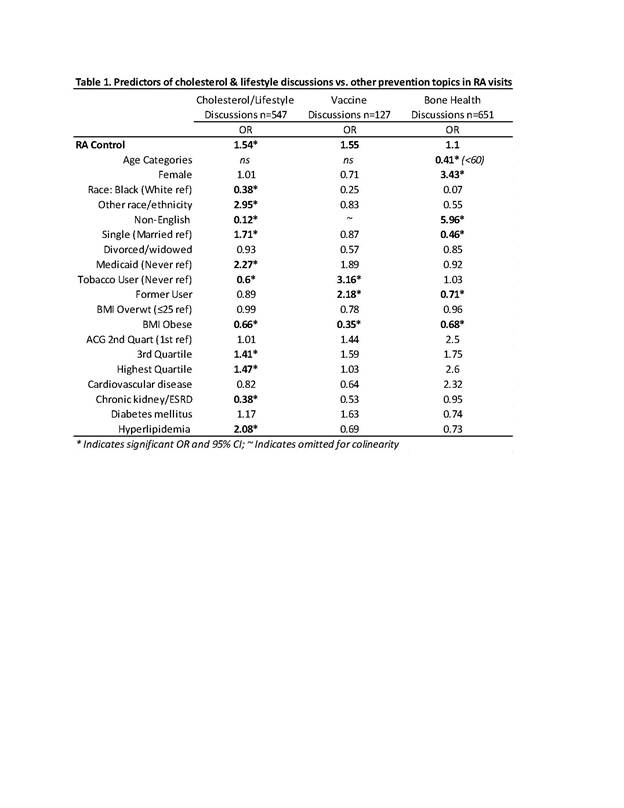
Results: 1785 abstracted RA visits showed a mean age 60 years, 84% female, 93% white, 10% smokers, and mean BMI was 30.2 (SD 7.3). Prevalent CVD was noted in 18%, diabetes 15%. Overall 37% of visits reported controlled RA, and 31% discussed either cholesterol or lifestyle (13% cholesterol). As hypothesized, perceived RA control at a visit increased the odds of cholesterol/lifestyle discussion at that visit (OR 1.54, 1.21-1.98; Table 1). Other predictors of cholesterol/lifestyle discussions included single marital status, Medicaid, higher ACG score and hyperlipidemia codes or medications. In contrast, black race, non-English language, tobacco use, obesity and chronic kidney disease (CKD) predicted lower odds of such discussions. RA control was not predictive of vaccine or bone health discussions which showed less variation. Obese patients had lower odds of any prevention discussions. Clinic effects were significant for cholesterol and vaccine discussions but not bone health (data not shown). Limitations of our study include a visit note level analysis, which may not reflect care over several visits or without documentation, and use of subjective “RA control” definitions, although this may reflect usual care.
Conclusion: Perceived RA control predicted higher odds of cholesterol/lifestyle discussions, but not vaccine or bone health discussions. Concerning low discussion rates in at-risk patients with tobacco use, obesity, chronic kidney disease, and black race and clinic variation call for improved quality guidelines and systematic practices to address modifiable CVD risk factors in RA visits.
Disclosure:
C. M. Bartels,
None;
J. Wong,
None;
H. Johnson,
None;
K. Voelker,
None;
M. Smith,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-cholesterol-and-lifestyle-discussions-in-rheumatoid-arthritis-visits-impact-of-perceived-ra-control-and-comparison-with-other-prevention-topics/