Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Costs in RA are substantial with 2-3 times higher mean annual costs than in the general population, but with a skewed cost distribution.[1] As a first step in identifying potential high cost patients, our aim was to identify predictors of costs, and assess the accuracy of prediction models in prevalent and incident RA patients using data from nationwide Swedish registers.
Methods: A prevalent cohort of RA patients ≥18y on Jan 1, 2010, was identified from the Swedish National Patient Register (requiring ≥2 visits listing RA) and the Swedish Rheumatology Quality Register, and followed until Dec 31, 2010. From the same registers, patients with the 1st visit listing RA in 2009, with a 2nd visit within one year, were identified to the incident cohort, and were followed for 1 year. Costs for inpatient care, nonprimary outpatient care, prescription drugs, and work loss, as well as explanatory variables, were retrieved from national registers. A linear regression model was used in a training set including 90% of the prevalent patients, and validated in the remaining 10%. The corresponding proportions in the smaller incident cohort were 50%/50%.
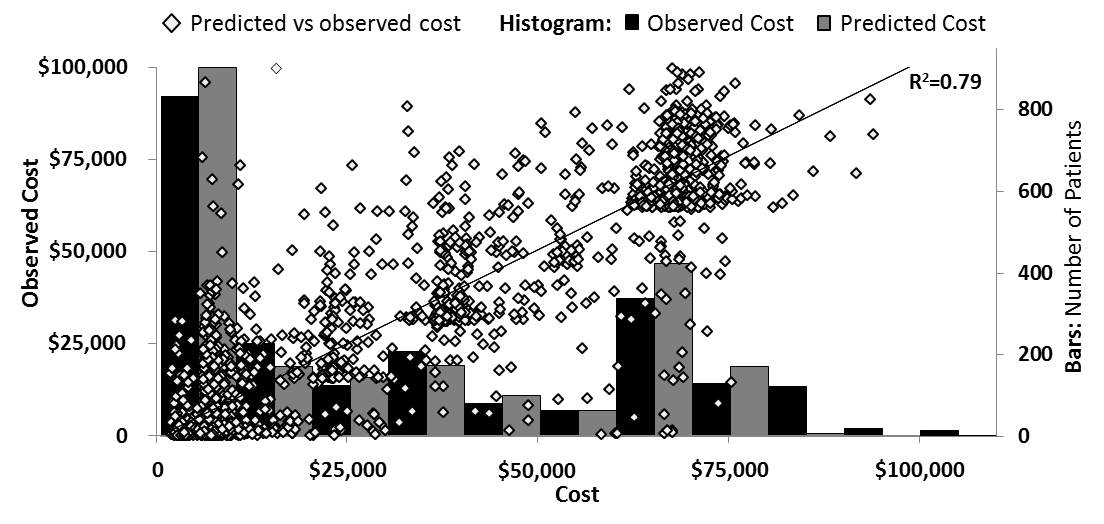
Results: 21,682 prevalent RA patients 18-64y were identified. The model included sex, age, time since register identification with RA, rheumatoid factor, hospital admission days and days of work loss the previous year, and any hospital admission/outpatient visit for chronic obstructive pulmonary disease, ischemic heart disease, and diabetes mellitus the previous 3 years. Predictions from the linear regression model performed well at the middle and higher end of the cost distribution, but poor in the lower cost segments (R2=0.79; Figure).
For the working age incident cohort (n=1378), the same variables were included plus annual income. Also this model performed better in the middle and higher cost segments than in the lower cost end of the distribution (R2=0.59).
In both models work loss days was the strongest predictor, where 1 more day of work loss the previous year was associated with a $165 (95%CI 163-166) higher annual cost in prevalent patients and $145 (95%CI 133-157) higher in incident patients. For patients ≥65y, a linear regression model including available variables from national data sources resulted in poor cost prediction (R2<0.15).
Conclusion: Reasonable prediction of annual costs in working age prevalent and incident RA patients was possible, while a satisfactory prediction model in older patients may need additional explanatory variables.
Reference
1. Eriksson J, et al. EULAR 2012; Abstract no: OP0121.
Figure Scatter plot and histogram of predicted vs observed costs in working age prevalent RA (n=2168)
Disclosure:
J. Eriksson,
None;
T. Frisell,
None;
J. Askling,
Pfizer Inc,
2;
M. Neovius,
Pfizer,
6.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-and-modeling-of-costs-in-rheumatoid-arthritis/