Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: About a quarter of pregnant individuals with systemic lupus erythematosus (SLE) have small for gestational age (SGA) infants. We aim to characterize placental pathology associated with SGA infants in SLE.
Methods: We retrospectively analyzed SLE deliveries who underwent placental analysis at UC San Diego from 11/2018-10/2023. We compared clinical and placental characteristics of SLE pregnancies that resulted in SGA to those that did not, and additionally, to a control group of matched pregnancies without SLE that resulted in SGA infants. Fisher’s exact and Mann-Whitney U tests were used to compare categorical and continuous variables, respectively.
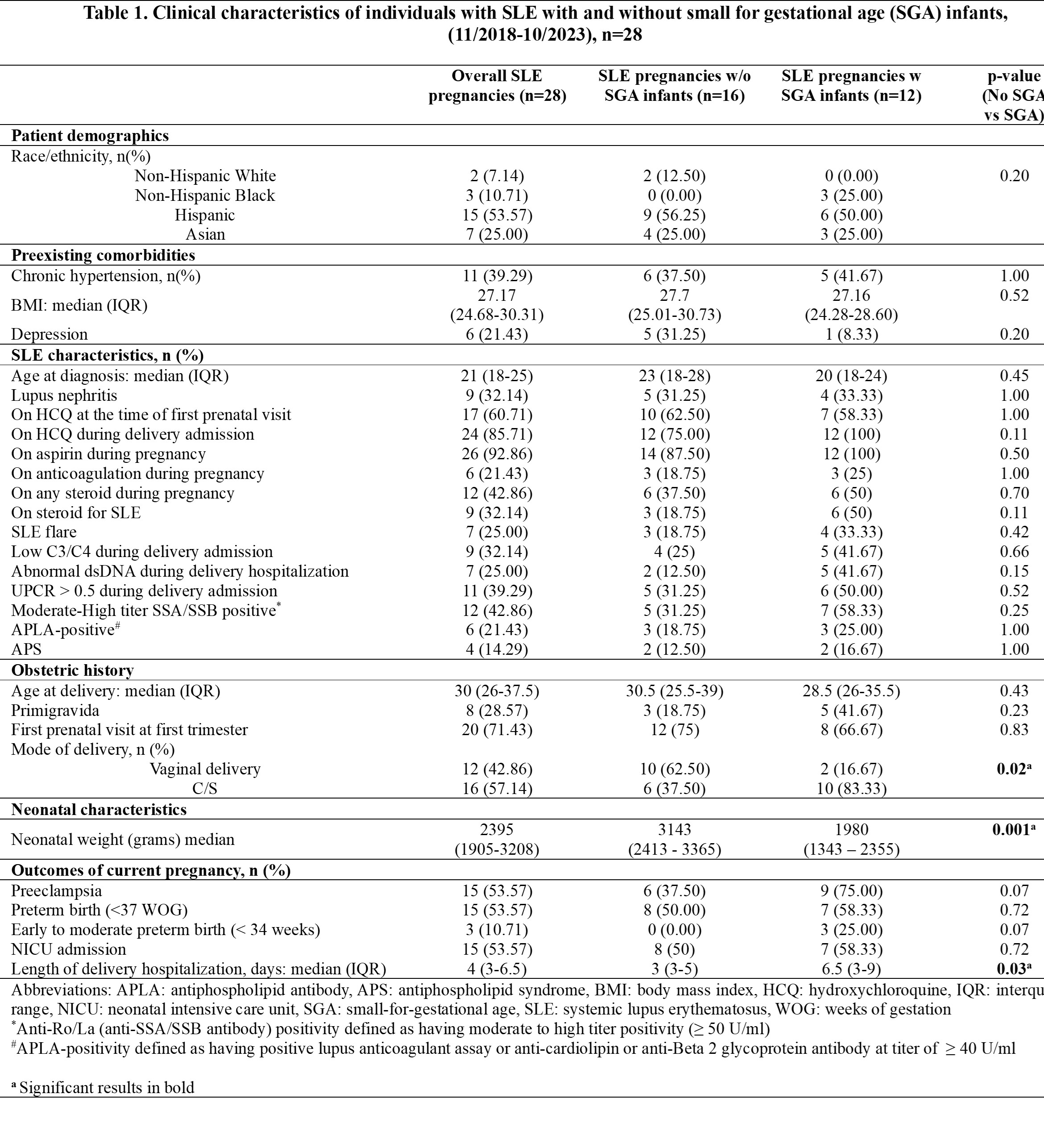
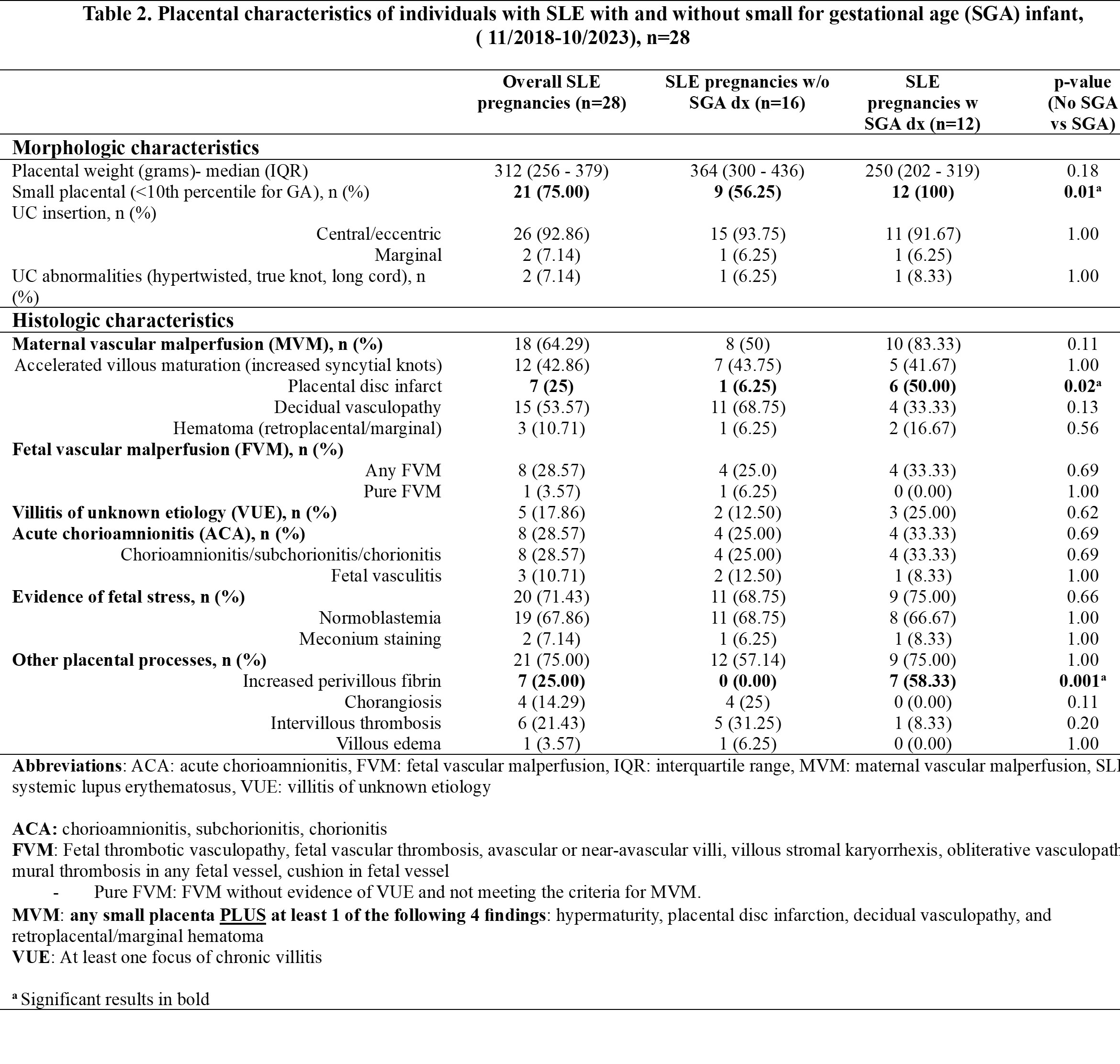
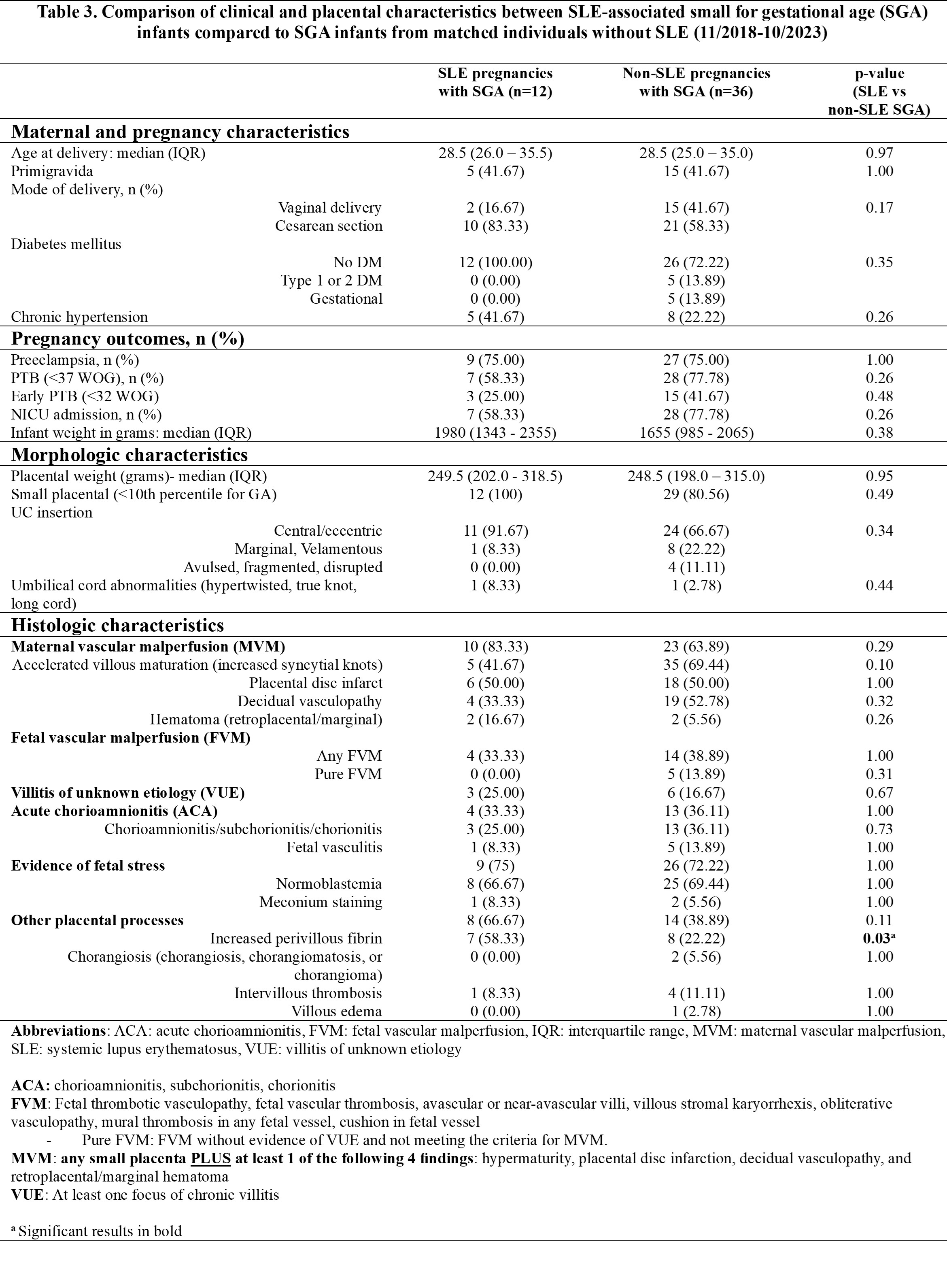
Results: Placental analysis was available for 28/70 (40%) SLE deliveries, which had a higher rate of adverse outcomes (75%) compared to 12% in those without placental analysis, and among these 28, all exhibited at least one placental abnormality (Table 1, Table 2). Twelve pregnancies resulted in SGA infants and 16 did not. Key placental findings distinguishing SLE pregnancies with SGA infants (vs. those without SGA) included small placental disc for gestational age (100% vs 56%, p = 0.01), placental disc infarct (50% vs 6%, p = 0.02), and increased perivillous fibrin deposition (PVFD, 58% vs 0%, p=0.001). Notably, 7/28 (25%) of studied SLE deliveries with available placental pathology exhibited increased PVFD, and all seven resulted in SGA infants (Table 2). Additionally, when compared to age- (±5 years) and gravidity- (primigravida vs non-primigravida) matched non-SLE pregnancies with SGA at a ratio of 3:1 (n=36), the only placental lesion that distinguished the two groups was a higher prevalence of increased PVFD in SLE-associated SGA cases (58% versus 22%, p = 0.03). The rate of placental disc infarct was similar in both groups (50%) (Table 3).
Conclusion: All 28 SLE deliveries with available placental pathology exhibited at least one histopathologic abnormality. Key placental features in SLE-associated SGA included small placenta, placental disc infarct, and increased PVFD. The occurrence of increased PVFD in placentas of SLE-associated SGA (58%) at a significantly higher rate compared to both SLE placentas without SGA (0%) as well as non-SLE placentas with SGA (22%) suggests that this lesion may represent a specific mechanism of placental injury leading to SGA in SLE. Increased PVFD has a reported prevalence of 0.09 – 2.7%, with a high recurrence rate (12-80%), and notable association with poor pregnancy outcomes (fetal deaths: 15 to 80 %, preterm births: 16.3-60% intrauterine growth restriction/SGA: 9 to >90%), which may be mitigated with the use of certain therapies. We propose that the presence of this lesion in the placenta, particularly in the setting of SGA, should warrant a closer look for potential underlying maternal autoimmune diseases, such as SLE.
(11/2018_10/2023), n=28
( 11/2018_10/2023), n=28
To cite this abstract in AMA style:
Dhital R, Jacobs M, Smith C, Parast M. Placental Characteristics in Systemic Lupus Erythematosus Pregnancies Resulting in Small for Gestational Age Infants [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/placental-characteristics-in-systemic-lupus-erythematosus-pregnancies-resulting-in-small-for-gestational-age-infants/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/placental-characteristics-in-systemic-lupus-erythematosus-pregnancies-resulting-in-small-for-gestational-age-infants/