Session Information
Session Type: ARP Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Physical activity can prevent and reduce depression, but there is little research on the relationship between physical inactivity and subsequent onset of depression in lupus. We examined physical inactivity as a predictor of incident depression in a cohort of individuals with SLE.
Methods: Data derive from the California Lupus Epidemiology Study (CLUES), a longitudinal cohort of 431 patients in the San Francisco Bay Area with confirmed SLE diagnoses, drawn from a variety of clinical sources and prior SLE studies. Participants complete an annual interview that includes sociodemographic questions and validated self-report measures of depression (Patient Health Questionnaire; PHQ-8), physical functioning (in Patient Reported Outcomes Measurement Information System; PROMIS), disease activity (Systemic Lupus Activity Questionnaire; SLAQ) and damage (Brief Index of Lupus Damage; BILD). A subset of participants also had physician assessed disease activity (SLE Disease Activity Index; SLEDAI) and damage (SLICC Damage Index; SDI). Physical inactivity was assessed at baseline from a single item: “I rarely or never do any physical activities.” Respondents were categorized as not depressed at baseline if their PHQ-8 scores were < 10, a validated cut-point. In that group, those with scores ≥ 10 in either of the next two annual interviews were considered to have incident depression. Using Cox proportional hazards regression, we modeled incident depression over a 2 year period as a function of baseline physical inactivity, controlling for sociodemographics, baseline physical functioning and disease status.
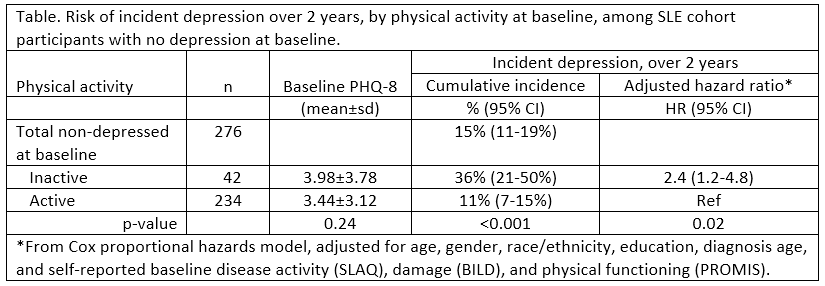
Results: 366 participants had ≥1 follow-up interview, of whom 256 (70%) had 2 follow-ups. At baseline, mean age of the sample was 47±14, 90% were female, 66% racial/ethnic minority. Among the 90 (25%) with PHQ-8 ≥10 at baseline, 33% were inactive vs. 16% of the 276 without baseline depression (p< 0.001). Those with baseline depression were excluded from further analysis. Mean PHQ scores for those without depression at baseline did not differ by activity status, but those who were inactive at baseline were more than 3 times as likely to develop depression over the next two years. After adjusting for baseline disease activity and damage (either by patient or physician assessment), physical function, and sociodemographics, the association remained moderately strong (hazard ratio, HR=2.4; see Table). Using physician assessed activity and damage reduced the sample size to 216 but did not appreciably change the results (HR=3.0; 95% CI= 1.4-6.7).
Conclusion: In this diverse cohort of patients with SLE, a simple question about low levels of physical activity was highly predictive of incident depression over the subsequent 2 years, after adjusting for sociodemographic and disease-related risk factors. Results support the importance of even low levels of physical activity and suggest an urgent need for approaches to increase physical activity in this high-risk patient population, such as health care providers’ recommendation of SLE-appropriate low impact activities (e.g., walking and swimming) and referral to community-based physical activity programs designed for individuals with SLE.
To cite this abstract in AMA style:
Trupin L, Patterson S, Murphy L, Dall'Era M, Yazdany J, Katz P. Physical Inactivity Is a Risk Factor for Incident Depression in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/physical-inactivity-is-a-risk-factor-for-incident-depression-in-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/physical-inactivity-is-a-risk-factor-for-incident-depression-in-systemic-lupus-erythematosus/